Cross-Species Pharmacokinetics: From Fundamental Principles to Model-Informed Drug Development
This article provides a comprehensive examination of comparative pharmacokinetics across species, a critical discipline for translational medicine and drug development.
Cross-Species Pharmacokinetics: From Fundamental Principles to Model-Informed Drug Development
Abstract
This article provides a comprehensive examination of comparative pharmacokinetics across species, a critical discipline for translational medicine and drug development. It explores the physiological and biochemical foundations of interspecies differences in drug absorption, distribution, metabolism, and excretion (ADME). The content details advanced methodological approaches including pharmacokinetic modeling, simulation, and allometric scaling for predicting human pharmacokinetics from preclinical data. Practical applications and case studies illustrate how these principles optimize dosing regimens, troubleshoot developmental challenges, and validate findings across species. Finally, the article addresses regulatory considerations and comparative validation strategies to enhance the reliability of interspecies extrapolations, providing researchers and drug development professionals with an integrated framework for more efficient and predictive drug development.
The Physiological Basis of Interspecies Pharmacokinetic Variability
Key Physiological Determinants of ADME Processes Across Species
In drug development, understanding the Absorption, Distribution, Metabolism, and Excretion (ADME) of compounds is fundamental to predicting their pharmacokinetic (PK) behavior and ultimate efficacy. These ADME processes are not uniform across different biological systems; they are profoundly influenced by species-specific physiological determinants. For researchers and drug development professionals, a clear, comparative understanding of these determinants is crucial for selecting appropriate animal models, extrapolating human pharmacokinetics, and reducing late-stage drug failures. This guide provides an objective comparison of key physiological factors affecting ADME across common research species, supported by experimental data and standardized protocols. The content is framed within the broader context of comparative pharmacokinetics, enabling more informed decision-making in preclinical research.
Core Physiological Determinants of ADME
The physiological factors governing a drug's journey through an organism can be broadly categorized by the ADME phase they most significantly impact. The following sections and tables summarize the key determinants and their species-specific variations.
Determinants of Absorption and Distribution
Absorption describes the process of a drug entering the systemic circulation, while distribution involves its movement throughout the body. Key physiological parameters influencing these phases include body composition, gastrointestinal physiology, and cardiovascular function [1] [2].
Table 1: Species Comparison of Physiological Factors Affecting Drug Absorption and Distribution
| Physiological Factor | Human | Rat/Mouse | Dog | Non-Human Primate | Impact on ADME |
|---|---|---|---|---|---|
| Body Fat Percentage | Variable (≈18-25%) | Lower (≈10-15%) | Variable by breed | Generally Lower | Affects volume of distribution for lipophilic drugs [2] |
| Plasma Volume & Albumin | ~3L; ~35-50 g/L | Much lower | Species-specific | Species-specific | Influences drug binding and free fraction available [1] |
| Gastrointestinal Transit Time | ~4-8 hours (small intestine) | Much faster (~2-4h) | Similar to human | Most similar to human | Impacts absorption window for orally administered drugs [2] |
| Gastric pH (Fasted) | ~1.5-2.0 | Highly variable | ~1.5-2.5 (dog) | Similar to human | Affects dissolution and stability of ionizable drugs [2] |
| Cardiac Output | ~5 L/min | Proportionally higher | Proportionally higher | Species-specific | Influences rate of drug distribution to tissues |
Determinants of Metabolism and Excretion
Metabolism involves the biochemical modification of a drug, primarily in the liver, and excretion is the process of eliminating the drug and its metabolites from the body, often via the kidneys or bile. Key determinants include the expression and activity of metabolizing enzymes and renal function [3] [2].
Table 2: Species Comparison of Physiological Factors Affecting Drug Metabolism and Excretion
| Physiological Factor | Human | Rat/Mouse | Dog | Non-Human Primate |
|---|---|---|---|---|
| Cytochrome P450 (CYP) Profile | CYP3A4 (major), 2D6, 2C9 | Different isoforms (e.g., Cyp3a, 2d) | CYP2B11, 2C21, 3A12 | Most similar profile to human |
| Liver Blood Flow | ~1.5 L/min | Proportionally much higher | Proportionally higher | Species-specific |
| Glomerular Filtration Rate (GFR) | ~125 mL/min | Proportionally higher | Proportionally higher | Closest to human |
| Biliary Function | Standard | More active (rodents) | Species-specific | Similar to human |
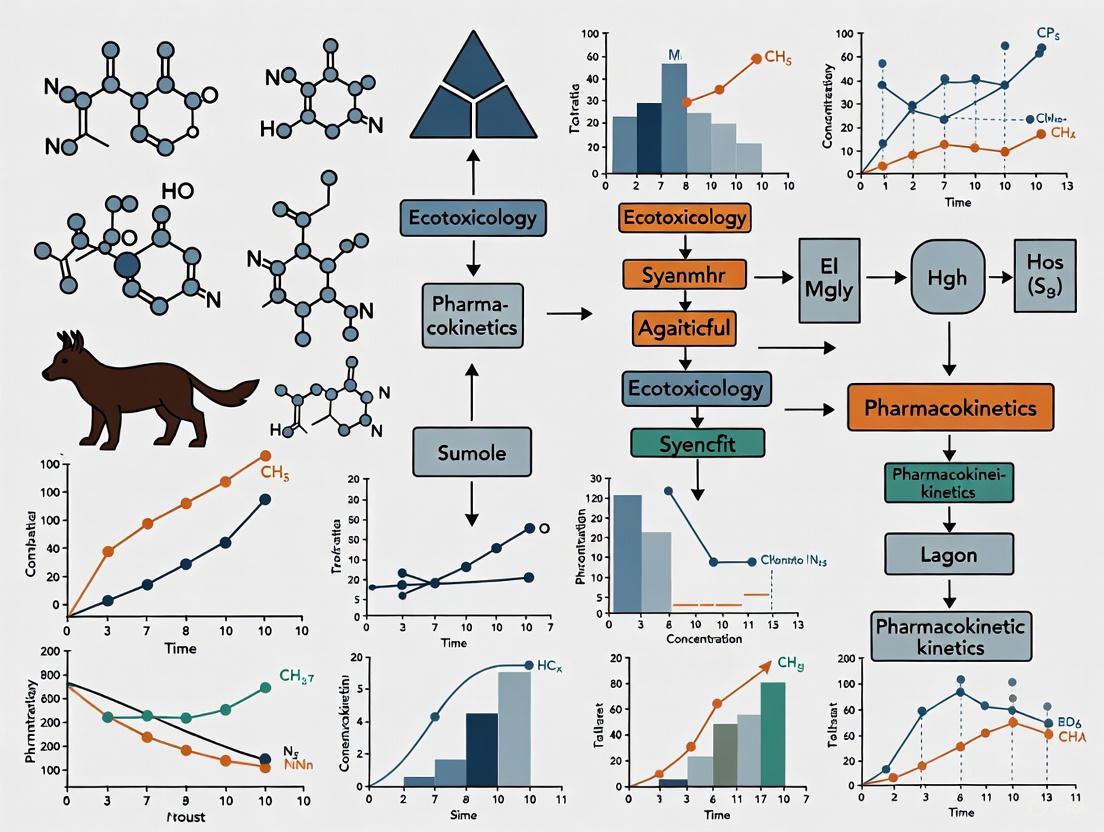
The relationships between these core physiological parameters and the resulting PK profile are complex. The following diagram illustrates the logical flow from a species' inherent physiology to its ADME characteristics.
Figure 1: The Logical Pathway from Physiology to Drug Efficacy. A species' physiological parameters directly determine the rates of ADME processes, which collectively define its pharmacokinetic profile and ultimately influence drug efficacy and toxicity.
Experimental Protocols for Assessing ADME Properties
Standardized experimental protocols are essential for generating reliable and comparable ADME data across species. The following section details key methodologies cited in the literature [2].
Lipophilicity Assessment (Log D)
Pharmacologic Question Addressed: "Will my parent compound be stored in lipid compartments or how well will it bind to a target protein?" Lipophilicity is a critical physicochemical property that influences solubility, absorption, membrane penetration, and distribution [2].
- Assay Design: The "shake-flask" method is the gold standard. Test articles are assayed in triplicate at one concentration (typically 10 µM) in a 1:1 mixture of n-octanol and aqueous buffer (pH 7.4). Positive (e.g., Testosterone) and negative (e.g., Tolbutamide) controls are included.
- Analysis: The concentration of the parent compound in each phase is measured using LC/MS/MS.
- Reporting: The result is reported as the Log D at pH 7.4, calculated as log([compound]~octanol~ / [compound]~buffer~).
- Compound Requirement: 1.0 - 2.0 mg.
Hepatic Microsome Stability
Pharmacologic Question Addressed: "How long will my parent compound remain circulating in plasma within the body?" This assay investigates the metabolic fate of compounds using subcellular liver fractions containing drug-metabolizing enzymes like cytochrome P450s (CYPs) [2].
- Assay Design: Test articles are incubated in triplicate with liver microsomes (e.g., 0.5 mg/mL from human, rat, or dog) at one concentration (typically 10 µM). Reactions are run with and without the cofactor NADPH to distinguish P450-mediated metabolism. Time points are taken at t = 0 and t = 60 minutes. A substrate with known activity (e.g., testosterone for CYP3A4) is used as a positive control.
- Analysis: LC/MS/MS is used to measure the remaining parent compound at each time point.
- Reporting: Data can be reported as a percentage of compound metabolized at a single time point or used to calculate intrinsic clearance and half-life with multiple time points.
- Compound Requirement: 1.0 - 2.0 mg.
Permeability Assays
Pharmacologic Question Addressed: "Will my compound be absorbed in the gastrointestinal tract?" Cell-based models like Caco-2 (human colon adenocarcinoma) are used to predict intestinal absorption.
- Assay Design: A monolayer of Caco-2 cells is grown on a permeable filter. The test compound is added to the donor compartment (apical for A->B transport, basolateral for B->A transport), and the amount appearing in the receiver compartment is measured over time.
- Analysis: LC/MS/MS is used to quantify the compound in both compartments. The apparent permeability (P~app~) is calculated.
- Reporting: Results are reported as P~app~ (A->B) for absorption potential and the efflux ratio (P~app~ (B->A) / P~app~ (A->B)) to identify substrates for efflux transporters like P-glycoprotein.
The workflow for a tiered ADME assessment strategy in early drug discovery is visualized below.
Figure 2: Tiered ADME Assessment Workflow. A two-tiered approach begins with rapid, cost-effective in vitro assays to screen compounds, followed by more resource-intensive in vivo pharmacokinetic studies for promising leads.
Essential Research Reagents and Tools
A robust ADME screening program relies on specific reagents, tools, and databases. The following table details key solutions used in the field [4] [2].
Table 3: Key Research Reagent Solutions for ADME Studies
| Research Reagent / Tool | Function / Application | Example Use-Case |
|---|---|---|
| Hepatic Microsomes | Subcellular liver fractions containing drug-metabolizing enzymes (CYPs, UGTs) for in vitro metabolism studies. | Assessing metabolic stability and identifying primary metabolic pathways in human, rat, dog, etc. [2] |
| Caco-2 Cell Line | A human colon cancer cell line that forms polarized monolayers, modeling the human intestinal barrier. | Predicting intestinal absorption and identifying efflux transporter substrates [2]. |
| Plasma/Serum | Sourced from various species for protein binding assays. | Determining the fraction of drug bound to plasma proteins, which influences free concentration and volume of distribution. |
| ADME Database | Specialized online databases (e.g., Fujitsu ADME Database) containing curated pharmacokinetic data. | Searching over 130,000 entries on metabolizing enzymes and transporters; comparing in vitro inhibition data with human clinical drug interaction data [4]. |
| CYP-Specific Probe Substrates | Compounds metabolized predominantly by a single cytochrome P450 enzyme (e.g., Testosterone for CYP3A4). | Serving as positive controls in enzyme activity and inhibition assays [2]. |
The physiological determinants of ADME processes vary significantly across species, presenting both a challenge and an opportunity for drug development researchers. A systematic, comparative understanding of factors such as body composition, organ function, and enzyme expression profiles is indispensable for selecting predictive animal models and for the accurate extrapolation of human pharmacokinetics. By employing standardized experimental protocols—such as microsomal stability and lipophilicity assays—and leveraging curated research tools and databases, scientists can generate robust, comparable data. This disciplined approach to comparative pharmacokinetics helps de-risk the drug development pipeline, ensuring that only the most viable candidate compounds, with ADME properties optimized for human therapeutic success, advance to clinical trials.
This guide objectively compares the anatomical and biochemical characteristics of digestive, metabolic, and excretory systems across species, providing supporting experimental data crucial for interspecies extrapolation in drug development.
Anatomical Comparisons of the Gastrointestinal Tract
The anatomical structure of the gastrointestinal (G.I.) tract directly influences drug dissolution, solubility, and transit times, causing significant variation in drug absorption from the oral route between humans and laboratory animals [5]. Key anatomical differences are summarized in Table 1.
Table 1: Comparative Gastrointestinal Anatomy and Physiology in Common Laboratory Animals and Humans [5]
| Species | Stomach pH | Primary Absorption Site | Colon pH | Transit Time (Hours) | Relative Length of G.I. Tract | Bile Flow (mL/kg/min) |
|---|---|---|---|---|---|---|
| Human | 1-2 (Fasted) | Small Intestine | 6-7 | 20-30 | Moderate | 1.4 - 5.3 |
| Mouse | 3-4 | Small Intestine | N/A | 5-11 | Short | 36.6 - 159 |
| Rat | 3-4 | Small Intestine | N/A | 12-24 | Moderate | 25.9 - 96.8 |
| Dog | 1-2 (Fasted) | Stomach, Small Intestine | 6-7 | 6-8 | Short | 4.5 - 19.3 |
| Monkey | 2-3 | Small Intestine | 6-7 | 15-24 | Moderate | 6.1 - 25.5 |
The G.I. tract is a continuous tube adapted for the sequential mechanical and enzymatic breakdown of food, with complexity increasing from simple organisms like sponges to more evolved mammals [6]. In higher animals, the tract features a two-opening system allowing continuous ingestion and excretion, significantly enhancing digestive efficiency [6]. Specialized structures, such as the small intestine, are critical for nutrient absorption, aided by features like villi that increase surface area [6].
The location and number of Peyer's patches, part of the gut-associated lymphoid tissue, can be important in the absorption of large molecules and particulate matter, varying significantly across species [5]. The lipid/protein composition of the enterocyte membrane along the G.I. tract can also alter binding and passive, active, and carrier-mediated transport of drugs [5].
Experimental Protocol: Assessing Drug Transit Time
Objective: To determine the transit time of an oral dosage form through the gastrointestinal tract in different animal species.
Methodology: [5]
- Administration: Animals are administered a radio-opaque marker or a stable, non-absorbable compound via oral gavage.
- Sampling: Feces are collected at predetermined time intervals post-administration.
- Analysis: The collected samples are analyzed for the presence of the marker. For radio-opaque markers, X-ray imaging can be used to track movement in real-time. For chemical markers, techniques like high-performance liquid chromatography (HPLC) are employed.
- Data Analysis: The transit time is calculated as the time taken for the first appearance of the marker in the feces. Data is presented as mean ± standard deviation for each group (n≥5).
Biochemical and Metabolic Comparisons
Drug metabolism is the processing of a drug by the body into subsequent compounds, primarily to convert it into more water-soluble substances for renal or biliary clearance [7]. The liver is the principal site of this metabolism, which typically inactivates drugs, though some metabolites are pharmacologically active [8].
Key Metabolic Pathways
Metabolism often occurs in two phases [7] [8]:
- Phase I Reactions (Functionalization): Involve formation of a new or modified functional group via oxidation, reduction, or hydrolysis. The most important enzyme system is cytochrome P-450 (CYP450).
- Phase II Reactions (Conjugation): Involve conjugation with an endogenous substance (e.g., glucuronic acid, sulfate, glycine) to make the drug more polar for excretion. Glucuronidation is the most common Phase II reaction.
Table 2: Key Drug-Metabolizing Enzymes and Their Activity Across Species [9] [8]
| Enzyme | Representative Substrate | Relative Activity in Common Species |
|---|---|---|
| CYP3A4 (Human) | Midazolam, Rivaroxaban | Human: High; Dog: Low; Rat: Moderate; Monkey: High |
| CYP2D6 (Human) | Tamoxifen, Bufuralol | Human: High (Polymorphic); Dog: Not significant; Rat: Moderate; Monkey: High |
| CYP2C9 (Human) | Warfarin, Phenytoin | Human: High; Dog: Low; Rat: Low; Monkey: Moderate |
| UGT (Glucuronidation) | SN-38 (Irinotecan metabolite) | Human: High; Cat: Deficient; Dog: Variable; Rat: High |
The following diagram illustrates the primary metabolic pathways and their localization within a hepatocyte.
Metabolism rates vary among individuals and species due to genetic factors, coexisting disorders, and drug interactions [8]. Most drugs follow first-order kinetics at therapeutic concentrations, but can saturate metabolic pathways and shift to zero-order kinetics at higher concentrations [8].
Experimental Protocol: Determining In Vitro Intrinsic Clearance
Objective: To estimate the intrinsic metabolic clearance (CL~int~) of a drug candidate using liver microsomes from different species. [9]
Methodology:
- Incubation: Liver microsomes (0.5 mg/mL protein) are incubated with the test compound (1 µM) in a potassium phosphate buffer (pH 7.4) containing NADPH (1 mM) as a cofactor. The reaction is carried out in a shaking water bath at 37°C.
- Sampling: Aliquots (50 µL) are taken from the incubation mixture at predetermined time points (e.g., 0, 5, 15, 30, 45, 60 minutes).
- Reaction Termination: The sampled aliquots are immediately added to a quenching solution (e.g., 100 µL of acetonitrile containing an internal standard) to stop the enzymatic reaction.
- Sample Analysis: Precipitated protein is removed by centrifugation, and the supernatant is analyzed using a validated LC-MS/MS method to determine the parent compound's concentration remaining at each time point.
- Data Analysis: The in vitro half-life (t~1/2~) and subsequently the CL~int~ are calculated from the slope of the natural logarithm of compound concentration versus time profile.
Advanced Modeling and Experimental Tools for Interspecies Extrapolation
Understanding physiological differences is critical for selecting the correct animal model to predict human bioavailability [5]. Two primary computational approaches are used for interspecies extrapolation.
Physiologically Based Pharmacokinetic (PBPK) Modeling
PBPK models incorporate species-specific physiological parameters (e.g., organ sizes, blood flows, tissue composition) to simulate drug concentration-time profiles in plasma and tissues. A study on the carcinogen Dibenzo[def,p]chrysene (DBC) developed a PBPK model that accurately predicted its disposition in both mice and humans, outperforming traditional allometric scaling [10]. Similarly, a minimal PBPK model for betamethasone successfully captured its pharmacokinetic profile across five species using a conserved partition coefficient and species-specific clearance values [11]. These models are also valuable for identifying complex processes like intestinal loss of a drug, which can be challenging to distinguish from hepatic first-pass metabolism [12].
The workflow for developing and applying a PBPK model is shown below.
Allometric Scaling
Allometric scaling is a simpler empirical approach that uses power laws based on body weight to extrapolate pharmacokinetic parameters across species. A meta-analysis of betamethasone pharmacokinetics found that its apparent clearance correlated reasonably well with body weight (power coefficient of 1.0, R² = 0.93) [11]. However, PBPK modeling often provides more accurate predictions, as it mechanistically accounts for species differences in physiology and biochemistry [10].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents for Comparative DMPK Studies
| Item | Function/Application |
|---|---|
| Liver Microsomes (Human & Animal) | In vitro system for studying Phase I metabolism and determining intrinsic clearance. [9] |
| Recombinant CYP450 Enzymes | Used to identify which specific CYP enzyme is responsible for metabolizing a drug candidate. [9] |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line used as an in vitro model of the human intestinal mucosa to study drug permeability and transport. [12] |
| Specific Enzyme Inhibitors (e.g., Ketoconazole) | Used in reaction phenotyping studies to chemically inhibit specific CYP enzymes and elucidate metabolic pathways. [8] |
| NADPH Regenerating System | Provides a constant supply of NADPH, a crucial cofactor for CYP450-mediated oxidative reactions. [8] |
| Ultrasensitive Analytical Techniques (e.g., AMS) | Accelerator Mass Spectrometry allows for measuring pharmacokinetics at environmentally relevant, low (nanomolar) doses, critical for toxicokinetic studies. [10] |
| Cryopreserved Hepatocytes | In vitro system that contains both Phase I and Phase II enzymes, providing a more complete model of hepatic metabolism than microsomes alone. [9] |
| Arisugacin C | Arisugacin C|Acetylcholinesterase Inhibitor|For Research |
| Cimicifugic Acid D | Cimicifugic Acid D|CAS 219986-51-3|Research Chemical |
Peptide therapeutics represent a rapidly growing class of pharmaceuticals that bridge the gap between small molecule drugs and large biologics. Defined as polymers of less than 50 amino acids with a molecular weight under 10 kDa, therapeutic peptides offer superior specificity in targeting molecular interactions compared to traditional small molecules, while typically exhibiting lower immunogenicity and manufacturing costs than protein-based biologics [13] [14]. However, their development faces significant pharmacological challenges, particularly concerning their pharmacokinetic properties and tissue distribution patterns (organotropism). Unmodified peptides generally undergo extensive proteolytic cleavage, resulting in short plasma half-lives, and their low permeability and susceptibility to catabolic degradation severely limit oral bioavailability [13].
Organotropism—the preferential distribution of therapeutic agents to specific tissues and organs—is a critical determinant of peptide drug efficacy and safety. For peptide therapeutics, distribution processes are mainly driven by a combination of diffusion and, to a lesser degree, convective extravasation, with volumes of distribution frequently not exceeding the volume of extracellular body fluid [13]. Understanding and optimizing organotropism is especially crucial for developing peptides that target central nervous system disorders, as they must traverse formidable biological barriers like the blood-brain barrier (BBB). This case study examines the comparative pharmacokinetics and organotropism of two research peptides, HAEE and HASS, within the broader context of species-dependent absorption, distribution, metabolism, and excretion (ADME) properties.
Comparative Pharmacokinetic Profiles of HAEE and HASS
HAEE Pharmacokinetics and Blood-Brain Barrier Penetration
HAEE (Acetyl-His-Ala-Glu-Glu-Amide) is a synthetic tetrapeptide analogue of the 35-38 region of the α4 subunit of α4β2 nicotinic acetylcholine receptor. Its primary therapeutic mechanism involves specific binding to the 11-14 site of Aβ, thereby reducing cerebral amyloidogenesis in Alzheimer's disease models [15]. Pharmacokinetic studies conducted in multiple laboratory animal species following single intravenous bolus administration have provided crucial insights into HAEE's distribution profile.
Key Pharmacokinetic Parameters of HAEE [15]
- BBB Penetration: Pharmacokinetic data provide direct evidence that HAEE crosses the blood-brain barrier.
- Mechanism of Brain Uptake: Molecular modeling suggests a role for LRP1 (Low-Density Lipoprotein Receptor-Related Protein 1) in receptor-mediated transcytosis of HAEE.
- Therapeutic Implication: The anti-amyloid effect of HAEE occurs due to its interaction with Aβ species directly in the brain parenchyma.
The ability of HAEE to cross the BBB represents a significant pharmacological advantage for CNS-targeting therapeutics, as this barrier prevents more than 98% of small molecules from entering the brain. The proposed LRP1-mediated transport mechanism is particularly significant, as this receptor is abundantly expressed at the BBB and plays a crucial role in transcytosing various ligands into the brain.
HASS Pharmacokinetics and Organotropism
Comprehensive pharmacokinetic data for the HASS peptide is currently limited in the available scientific literature. This significant gap in research presents challenges for direct comparison with HAEE's established organotropic profile. Future studies should prioritize characterizing HASS's absorption, distribution, metabolism, and excretion patterns, with particular emphasis on its potential for CNS penetration compared to HAEE.
Comparative Pharmacokinetic Table
Table 1: Comparative Pharmacokinetic Parameters of HAEE and HASS Peptides
| Parameter | HAEE | HASS | Methodological Notes |
|---|---|---|---|
| Blood-Brain Barrier Penetration | Demonstrated in multiple animal models [15] | Insufficient data | Assessed via pharmacokinetic modeling and molecular docking |
| Proposed Transport Mechanism | LRP1-mediated transcytosis [15] | Insufficient data | Molecular modeling suggests receptor-mediated transport for HAEE |
| Primary Molecular Target | Aβ (11-14 site) [15] | Insufficient data | Surface plasmon resonance and binding assays confirm HAEE-Aβ interaction |
| Therapeutic Application | Alzheimer's disease (anti-amyloid) [15] | Insufficient data | Demonstrated in transgenic mouse models of Alzheimer's |
| Key Metabolic Challenges | Susceptibility to proteolytic degradation [13] | Insufficient data | Peptides generally vulnerable to ubiquitous proteases/peptidases |
Experimental Protocols for Assessing Peptide Organotropism
In Vivo Pharmacokinetic and Biodistribution Studies
Animal Models and Dosing
- Species Selection: Studies should incorporate multiple species (typically rats and rabbits) to identify interspecies differences in peptide metabolism and distribution [16].
- Dosing Administration: Peptides are administered via single intravenous bolus injection into the caudal vein for precise pharmacokinetic profiling [17].
- Dose Selection: Doses should be calculated based on prior efficacy studies and radiolabeling requirements for accurate detection.
Sample Collection and Analysis
- Blood Sampling: Serial blood samples are collected at predetermined time points (e.g., 1, 5, 15, 30, 60, 120, 240 minutes post-injection) via indwelling catheters [17].
- Plasma Separation: Blood samples are immediately centrifuged (e.g., 5,000 × g for 10 minutes at 4°C) to obtain plasma.
- Tissue Collection: At terminal time points (e.g., 1 hour and 5 hours post-injection), target organs (brain, liver, spleen, kidneys, lungs, heart, muscle) are harvested, weighed, and homogenized [17].
- Radiolabel Detection: For radiolabeled peptides (e.g., tritium-labeled), tissue and plasma samples are analyzed using liquid scintillation counting to quantify peptide concentrations [17].
- Data Analysis: Non-compartmental analysis is performed to determine standard pharmacokinetic parameters (Cmax, Tmax, AUC, t1/2, Vd, Cl). Tissue distribution is expressed as volume of distribution (VD) by dividing radioactivity in each organ (dpm/g) by plasma radioactivity (dpm/μl) [17].
Blood-Brain Barrier Penetration Assessment
In Situ Cerebral Perfusion (ISCP)
- Surgical Preparation: Animals are anesthetized, and the common carotid arteries are exposed and cannulated.
- Perfusion Technique: Buffer containing the test peptide is perfused through the carotid artery at a constant flow rate for a predetermined period (e.g., 30-60 seconds) [17].
- Brain Collection: Immediately after perfusion, animals are decapitated, and the ipsilateral hemisphere is collected.
- Uptake Quantification: The brain uptake coefficient (µl gâ»Â¹ sâ»Â¹) is calculated to quantify BBB permeability [17].
- Barrier Integrity Assessment: Inclusion of integrity markers (e.g., sucrose, inulin) confirms BBB remains intact during the experiment.
Molecular Modeling of Transport Mechanisms
- Receptor Docking Studies: Computational modeling predicts interactions between peptide candidates and BBB receptors (e.g., LRP1) [15].
- Structure-Activity Relationship (SAR) Analysis: Systematic amino acid substitutions identify structural determinants of BBB penetration.
Table 2: Key Research Reagent Solutions for Peptide Organotropism Studies
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Radiolabeled Compounds | ³H-labeled peptides | Enable precise tracking and quantification of peptides in biological matrices via scintillation counting [17] |
| BBB Integrity Markers | ¹â´C-sucrose, ³H-inulin | Assess blood-brain barrier integrity during penetration studies [17] |
| Metabolic Stabilizers | Protease/peptidase inhibitors | Prevent ex vivo degradation of peptides during sample processing [13] |
| Molecular Modeling Tools | Docking software (AutoDock, Schrödinger) | Predict peptide-receptor interactions and transport mechanisms at biological barriers [15] |
| Chromatographic Systems | HPLC/UPLC with mass spectrometry | Separate and quantify peptides and their metabolites in complex biological samples [16] |
Experimental Workflow Diagram
Diagram 1: Experimental workflow for evaluating peptide organotropism and BBB penetration.
Species Differences in Peptide Pharmacokinetics
Interspecies variation significantly impacts the pharmacokinetic profiles of therapeutic peptides, creating challenges in translational research. Comparative studies in rats and rabbits reveal substantial differences in metabolic handling of peptide therapeutics, primarily attributed to variations in gastrointestinal esterases and peptidases [16]. These enzymatic differences directly influence organotropism by altering systemic exposure and tissue distribution patterns.
Key Species-Specific Metabolic Considerations [16]
- Rat Models: Exhibit intensive first-pass metabolism of ester-containing peptides via gastrointestinal esterases and peptidases, generating active metabolites but reducing parent compound bioavailability.
- Rabbit Models: Demonstrate lower enzymatic activity toward peptide substrates, resulting in prolonged plasma detection and potentially altered tissue distribution profiles.
- Structural Determinants: Ester derivatives (e.g., noopept, dilept) undergo more extensive hydrolysis than amide derivatives (e.g., GB-115), with the latter demonstrating greater metabolic stability across species.
- Translation Implications: Species selection critically influences pharmacokinetic parameters and must be carefully considered when extrapolating organotropism data to humans.
These interspecies differences extend beyond metabolism to include variations in hepatic and renal blood flow, protein binding, and tissue-specific uptake mechanisms—all factors that collectively determine organotropism. Understanding these differences is essential for designing appropriate preclinical studies and predicting human pharmacokinetics.
This comparative analysis highlights the critical importance of organotropism in developing effective peptide therapeutics, using HAEE as a model for CNS-targeting peptides with demonstrated blood-brain barrier penetration capabilities. The significant research gap regarding HASS pharmacokinetics underscores the need for systematic evaluation of its absorption, distribution, metabolism, and excretion properties, particularly its potential for brain penetration relative to HAEE.
The translational value of organotropism studies depends heavily on careful consideration of species-specific metabolic differences and the application of rigorous experimental methodologies, including radiolabeled distribution studies and specialized BBB penetration assessments. Future research should prioritize structural-activity relationship studies to identify molecular determinants of desirable tissue distribution patterns, potentially enabling rational design of peptides with optimized organotropism for specific therapeutic applications.
As peptide therapeutics continue to expand into new disease areas, including metabolic disorders, oncology, and infectious diseases, understanding and controlling their tissue distribution will remain fundamental to developing safe and effective treatments. The methodologies and considerations outlined in this case study provide a framework for such investigations, emphasizing the integration of pharmacokinetic principles with therapeutic objectives.
Impact of Genetic Polymorphisms on Drug Metabolism and Disposition
Genetic polymorphisms significantly influence interindividual variability in drug metabolism and disposition, impacting both drug efficacy and safety. These variations in genes encoding drug-metabolizing enzymes and transporter proteins can alter pharmacokinetic parameters, leading to differential drug responses among patients and across species. Understanding these differences is critical in drug development and clinical practice, as it aids in predicting drug behavior, optimizing dosing regimens, and minimizing adverse drug reactions. This guide compares the impact of key genetic polymorphisms on drug metabolism and disposition, providing experimental data and methodologies relevant to researchers and drug development professionals.
Key Genetic Polymorphisms Affecting Drug Metabolism
Genetic polymorphisms in genes coding for cytochrome P450 (CYP) enzymes and drug transporters are major contributors to variability in drug pharmacokinetics. The tables below summarize the effects of major polymorphisms.
Table 1: Major Cytochrome P450 Polymorphisms and Clinical Impact
| Enzyme | Key Substrates | Variant Alleles | Functional Effect | Clinical Consequence |
|---|---|---|---|---|
| CYP2C9 | S-warfarin, phenytoin, fluvastatin [18] [19] | *2, *3 [19] | Reduced enzymatic activity [19] | Reduced drug clearance; increased risk of toxicity (e.g., bleeding with warfarin) [19] |
| CYP2C19 | Clopidogrel, proton pump inhibitors, voriconazole [20] | *2, *3 (Poor Metabolizers), *17 (Ultrarapid) [19] [20] | Deficient/Reduced or Increased activity [19] | Poor metabolizers: reduced activation of clopidogrel [20]. Ultrarapid metabolizers: therapeutic failure with omeprazole [19]. |
| CYP2D6 | Codeine, tamoxifen, tricyclic antidepressants [19] [20] | *3, *4, *5, *6 (Poor Metabolizers) [19] | Enzyme activity from deficient to ultrarapid [19] | Poor metabolizers: poor analgesic effect of codeine. Ultrarapid metabolizers: potential for toxicity [19]. |
| CYP3A5 | Tacrolimus [20] | *3 [20] | Reduced metabolism | Altered drug exposure requiring dose adjustment [20] |
Table 2: Key Drug Transporter Polymorphisms and Clinical Impact
| Transporter | Gene | Key Substrates | Key Polymorphism | Functional & Clinical Impact |
|---|---|---|---|---|
| OATP1B1 | SLCO1B1 | Statins (fluvastatin, simvastatin) [18] [20] | T521C (rs4149056) [18] | Reduced hepatic uptake; associated with increased systemic exposure and risk of statin-induced myopathy [18] [20] |
| P-glycoprotein | ABCB1 (MDR1) | Digoxin, cyclosporine, paclitaxel [21] | C3435T, G2677T/A [18] [21] | Altered drug absorption and distribution; influenced pharmacokinetics of drugs like indinavir and digoxin [21] |
| BCRP | ABCG2 | Rosuvastatin [20] | C421A [18] [20] | Reduced transport; increased plasma concentrations of substrates [20] |
Experimental Protocols for Pharmacogenetic Analysis
Clinical Study Design for Assessing Fluvastatin Pharmacogenetics
A typical clinical protocol to investigate the effect of genetic polymorphisms on drug pharmacokinetics involves a controlled crossover design [18].
- Study Population: Recruit healthy subjects (e.g., n=24), with health status confirmed by medical history, physical examination, and laboratory tests. Obtain written informed consent and ethical approval [18].
- Study Design: Open-label, randomized, two-period, two-treatment crossover study. For example:
- Treatment A: Fluvastatin 40 mg immediate-release (IR) capsule twice daily for 7 days.
- Treatment B: Fluvastatin 80 mg extended-release (ER) tablet once daily for 7 days.
- Include a washout period (e.g., one week) between treatment periods [18].
- Blood Sampling: Collect serial blood samples (e.g., 3.5 ml) at multiple time points following drug administration on Day 1 (single dose) and Day 7 (steady state). For an ER formulation, samples may be taken at 0, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 10, 12, 16, and 24 hours. For a twice-daily IR formulation, sampling is more frequent around both doses [18].
- Sample Processing: Centrifuge blood samples to separate serum. Store serum samples at -70°C until analysis [18].
- Genotyping: Genotype participants for relevant polymorphisms (e.g., SLCO1B1 T521C, CYP2C93, CYP3A53, ABCB1, ABCG2) using validated methods [18].
- Data Analysis:
- Use HPLC-MS/MS to determine serum drug concentrations [18].
- Calculate pharmacokinetic parameters (e.g., AUC~0-24~, C~max~, T~max~, t~1/2~).
- Employ statistical models (e.g., ANOVA, nonlinear mixed-effects models) to analyze the effect of genotype on PK parameters, accounting for factors like formulation and dosing day [18] [21].
In Vitro Transporter Kinetics Assay
In vitro studies help mechanistically confirm clinical findings, such as the impact of the SLCO1B1 T521C polymorphism on fluvastatin uptake [18].
- Cell Culture: Maintain engineered cell lines, such as HEK293 cells stably transfected with reference (SLCO1B1 521TT) or variant (SLCO1B1 521CC) transporter [18].
- Uptake Experiment:
- Grow cells to confluence in appropriate media (e.g., DMEM with FBS and antibiotics).
- Incubate cells with varying concentrations of the drug of interest (e.g., fluvastatin from <1 µmol/L to >1 µmol/L) for a defined period.
- Terminate the uptake process by washing cells with cold buffer.
- Lyse cells and analyze drug concentration inside the cells using a sensitive method like LC-MS/MS.
- Data Analysis:
- Determine kinetic parameters (K~m~, V~max~) for the transporter in both reference and variant cell lines.
- Compare uptake velocities at different substrate concentrations to understand how polymorphism affects function, especially at low vs. high drug concentrations [18].
Visualization of Pharmacogenetic Relationships
The following diagram illustrates the core workflow and relationships between genetic polymorphisms, their functional consequences, and the resulting clinical outcomes.
Figure 1: Pathway from genetic polymorphism to clinical outcome, showing how variants in genes like CYP450s or transporters alter function, leading to changes in pharmacokinetics (PK) and ultimately impacting patient response.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for Pharmacogenetic Research
| Reagent / Resource | Function / Application | Examples / Specifications |
|---|---|---|
| Transfected Cell Models | In vitro study of transporter function and kinetics. | HEK293 or CHO cells stably expressing variant (e.g., SLCO1B1 521CC) or reference transporters [18]. |
| Clinical DNA Samples | Genotyping and correlation with pharmacokinetic data. | DNA extracted from participants in clinical trials, with informed consent for pharmacogenetic analysis [18]. |
| LC-MS/MS System | Sensitive and specific quantification of drug concentrations in biological matrices (serum, cell lysates). | HPLC system (e.g., Waters Xterra MS C18 column) coupled to a mass spectrometer (e.g., API4000) [18]. |
| Pharmacogenetic Databases | Curated evidence for gene-drug relationships and clinical implementation guidelines. | PharmGKB, Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines [22] [23] [20]. |
| Statistical Software | Analysis of genotype-PK relationships using population PK modeling or hypothesis testing. | NONMEM, R, or other software for ANOVA on EBEs or likelihood ratio tests in mixed-effects models [21]. |
| Memnobotrin A | Memnobotrin A, MF:C25H33NO5, MW:427.5 g/mol | Chemical Reagent |
| Fudecalone | Fudecalone | Research-grade Fudecalone, a synthetic drimane terpenoid with anticoccidial activity. For Research Use Only. Not for human or veterinary use. |
Cross-Species Comparisons in Pharmacokinetics
Understanding species differences is fundamental to extrapolating animal data to humans in drug development. While the basic structure of biomembranes and absorption processes are similar across mammals, significant differences exist in metabolism and excretion [24] [25].
- Absorption: The intrinsic absorption of a drug across the gastrointestinal epithelium is generally similar among species. However, factors like gastric pH, GI tract anatomy (ruminant vs. non-ruminant), and first-pass metabolism can vary considerably, leading to species differences in overall oral bioavailability [24] [25] [26].
- Metabolism: This is a major source of interspecies variation. Cytochrome P450 enzymes and other metabolizing systems have different expression levels, substrate specificities, and catalytic activities across species [24] [25] [26]. For example, the high rate of oxidative metabolism in mice can make them poor models for chronic human toxicity studies [26].
- Elimination: Renal excretion can be predicted with relative success using allometric scaling based on glomerular filtration rates. In contrast, hepatic clearance limited by metabolism is less predictable due to the biochemical variability of drug-metabolizing enzymes [24].
Cardiovascular and Body Composition Differences and Their PK Implications
In the field of comparative pharmacokinetics (PK), understanding the interplay between cardiovascular physiology, body composition, and drug disposition is paramount for translating findings from nonclinical models to human patients. Significant differences in body structure and cardiovascular function between species, and between individuals within a species, introduce substantial variability in the absorption, distribution, metabolism, and excretion (ADME) of pharmaceutical compounds [27]. The rising prevalence of polypharmacy further amplifies this challenge, increasing the risk of drug-drug interactions (DDIs) that can alter drug exposure and compromise therapeutic efficacy or safety [28]. This guide objectively compares the influence of cardiovascular and body composition factors on PK parameters across research models, providing a structured overview of key experimental data and methodologies essential for drug development professionals.
Body Composition Parameters and Their Pharmacokinetic Relevance
Body composition—the relative proportions of fat, muscle, bone, and water in the body—profoundly influences drug pharmacokinetics. Key parameters provide predictive value for cardiometabolic risk and drug disposition.
Table 1: Body Composition Assessment Methods and PK Implications
| Assessment Method | Measured Parameters | Pharmacokinetic Implications | Key Research Findings |
|---|---|---|---|
| Waist Circumference [29] | Abdominal adiposity | Altered volume of distribution ((V_d)) for lipophilic drugs; modified drug clearance. | Recommended thresholds: ≤37 inches (men), ≤32 inches (women). Exceeding these indicates higher cardiometabolic risk [29]. |
| Waist-to-Hip Ratio [29] | Fat distribution pattern ("apple" vs. "pear" shape) | Influences drug distribution and metabolism; apple shape (higher ratio) linked to greater PK variability. | A ratio where waist > hips indicates higher risk for weight-related health issues and potential alterations in drug response [29]. |
| Body Fat Percentage (BFP) [29] | Proportion of total mass as fat | Higher BFP increases (V_d) and half-life for lipophilic drugs; can delay onset and prolong duration of action [30]. | Healthy ranges: 8-19% (men), 21-33% (women). Higher percentages correlate with cardiovascular disease risk [29]. |
| AI-MRI Analysis [31] | Visceral Adipose Tissue (VAT), Skeletal Muscle (SM) proportion, Skeletal Muscle Fat Fraction (SMFF) | VAT and SMFF are independent predictors of metabolic dysfunction, potentially affecting hepatic drug metabolism and systemic clearance. | High VAT and SMFF associated with increased diabetes (aHR: 2.16 women, 1.84 men) and major adverse cardiovascular event (MACE) risk after adjusting for BMI [31]. |
| Bio-impedance Analysis (BIA) [32] | Fat-free mass (FFM), Fat mass (FM), Basal Metabolic Rate (BMR) | FFM and BMR are key determinants of drug clearance; lower FFM may correlate with reduced metabolic capacity. | Studies show body composition (BMI, FFM, BMR) significantly influences cardiorespiratory fitness, an indirect marker of overall metabolic health and drug clearance capacity [32]. |
Cardiovascular and Gender Differences in Drug Response
Significant gender-related differences in cardiovascular physiology and pharmacology exist, driven by variations in body composition, hormone levels, and metabolizing enzymes.
Table 2: Gender Differences in Cardiovascular Drug Pharmacokinetics and Effects
| Drug Class | Documented Gender Difference | Postulated Mechanism |
|---|---|---|
| Beta-Blockers (e.g., Metoprolol, Propranolol) [30] | Higher plasma levels in women; slower clearance; greater reduction in exercise heart rate and systolic blood pressure. | Slower clearance and lower volume of distribution in women, potentially due to body composition differences. |
| Statins [30] | Generally higher plasma concentrations in women. | Body size and composition differences; women have higher CYP3A4 concentrations, affecting metabolism of lipophilic statins. |
| Anticoagulants (Warfarin) [30] | Women typically require lower doses for therapeutic INR. | Influenced by protein binding and exogenous sex hormones. |
| Digoxin [30] | Associated with increased risk of death in women with heart failure. | Not fully elucidated; may be related to dosing relative to body size rather than intrinsic PK differences. |
| Calcium Channel Blockers (e.g., Verapamil) [30] | Increased clearance observed in women. | Not fully specified; potentially due to gender-specific metabolic pathways. |
Underlying these pharmacological differences are fundamental physiological disparities. Females generally have higher body fat percentages, influencing the distribution of lipophilic drugs [30]. They also exhibit distinct hemodynamic regulation, including lower vascular resistance and a blunted sympathetic response during physical exertion compared to males [33]. Furthermore, hepatic drug clearance is often lower in women, impacting the metabolism of numerous cardiovascular medications [30]. These factors collectively contribute to the higher incidence of certain adverse drug reactions, such as drug-induced torsades de pointes, in women [30].
Experimental Protocols for Assessing Body Composition and Cardiovascular Function
AI-Based Body Composition Analysis from MRI
The automated analysis of body composition from whole-body MRI scans represents a advanced methodological approach.
- Objective: To derive accurate 3D measurements of body composition compartments (VAT, SAT, SM, SMFF) and assess their association with cardiometabolic outcomes [31].
- Procedure:
- Subject Preparation: Participants undergo whole-body MRI scanning according to standard institutional protocols.
- Image Acquisition: High-resolution MRI images are obtained.
- AI Analysis: An artificial intelligence tool is applied to the MRI DICOM data to automatically segment and quantify different tissue types.
- Data Calculation: The relative proportions of subcutaneous adipose tissue (SAT), visceral adipose tissue (VAT), skeletal muscle (SM), and skeletal muscle fat fraction (SMFF) are calculated.
- Statistical Analysis: Associations between these composition measures and incident diabetes or major adverse cardiovascular events (MACE) are evaluated using multivariate Cox proportional hazards models, adjusting for confounders like age, smoking, and hypertension [31].
- Key Outputs: Hazard ratios (aHR) for disease outcomes per standard deviation increase in body composition metric; quantification of the proportion of the population in high-risk categories (e.g., top 5th percentile for VAT) [31].
Cardiorespiratory Fitness (CRF) Assessment via Balke Treadmill Test
The Balke treadmill protocol is a standardized method to assess maximal oxygen uptake (VOâ‚‚ max), a gold-standard measure of cardiorespiratory fitness.
- Objective: To determine maximal oxygen uptake (VOâ‚‚ max) as a primary indicator of cardiorespiratory fitness and cardiovascular health [32].
- Procedure:
- Subject Preparation: Participants are asked to abstain from eating or drinking for 4-5 hours prior to testing. Pre-test anthropometric measurements (height, weight) and body composition (via bio-impedance analyzer) are taken [32].
- Baseline Measurements: Resting heart rate (HR), blood pressure (BP), and respiratory rate (RR) are recorded.
- Exercise Protocol: The participant walks on a treadmill at a constant speed with incremental grade increases (typically 1% per minute) until volitional exhaustion.
- Monitoring: HR, BP, and RR are monitored throughout the test. The test is terminated if the participant experiences excessive fatigue or distress.
- Calculation: VO₂ max is calculated using the formula: VO₂ max = 1.38 × T + 5.22, where "T" is the total test time in minutes and fractions of a minute [32].
- Key Outputs: VOâ‚‚ max value (mL/kg/min); correlation data between VOâ‚‚ max and body composition parameters like BMI and body fat percentage [32].
High-Intensity Interval Training (HIIT) Intervention Study
This protocol examines individual variability in response to exercise, linking changes in body composition to cardiovascular and cardiorespiratory adaptations.
- Objective: To investigate cardiovascular and cardiorespiratory adaptations to exercise in individuals showing different levels of responsiveness to changes in body fat percentage (BFP) [34].
- Procedure:
- Participant Recruitment: Adolescents or adults are recruited and randomly assigned to experimental or control groups.
- Pre-intervention Testing: Baseline measurements of BFP (using a validated analyzer like InBody230), resting BP, and CRF (e.g., VOâ‚‚ max) are collected.
- Intervention: The experimental group undergoes a structured HIIT program (e.g., 10 weeks of school-based HIIT during physical education lessons). The control group continues with standard activities.
- Post-intervention Testing: All baseline measurements are repeated after the intervention period.
- Data Analysis: Participants are classified as Responders (RsBFP) or Non-Responders (NRsBFP) based on their change in BFP. Pre- and post-intervention BP and CRF are compared between these groups to determine if body fat changes correlate with cardiovascular benefits [34].
- Key Outputs: Mean change in BFP, systolic BP, and CRF in RsBFP vs. NRsBFP; statistical analysis of interaction effects (e.g., via ANOVA) [34].
Visualization of Pathways and Workflows
Body Composition Impact on Pharmacokinetics
- Title: Body Composition Impact on PK
Experimental Body Composition Workflow
- Title: Experimental Body Composition Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Body Composition and PK Research
| Tool/Reagent | Primary Function | Application Example | Key Features |
|---|---|---|---|
| Bio-impedance Analyzer (BIA) [32] | Measures body composition (FFM, FM, BFP, BMR) via electrical impedance. | Prospective cross-sectional studies linking body composition to cardiorespiratory fitness (VOâ‚‚ max) [32]. | Non-invasive; provides rapid estimates of multiple body composition parameters. |
| Whole-Body MRI with AI Software [31] | Provides precise 3D volumetric quantification of body compartments (VAT, SAT, SM). | Large-scale cohort studies to establish associations between specific fat/muscle deposits and cardiometabolic risk [31]. | High accuracy; enables opportunistic assessment from routine clinical images; automated analysis. |
| Body Composition Analyzer (e.g., InBody230) [34] | Directly measures body weight, BFP, fat mass, and fat-free mass. | Monitoring changes in body fat percentage in response to exercise interventions (e.g., HIIT studies) [34]. | High reliability (ICC ≥ 0.98); essential for classifying treatment responders vs. non-responders. |
| Automated Blood Pressure Monitor [34] | Measures resting systolic and diastolic blood pressure. | Assessing cardiovascular adaptations and safety endpoints in intervention studies and clinical trials [34]. | Standardized, non-invasive cardiovascular assessment. |
| Human Liver Microsomes (HLMs) [28] | In vitro system containing human CYP enzymes for drug metabolism studies. | Reaction phenotyping to identify enzymes responsible for drug metabolism and assess DDI potential [28]. | Critical for predicting metabolic clearance and enzyme-mediated DDIs in early drug development. |
| Recombinant Human Enzyme (RHE) Systems [28] | Engineered cell systems expressing specific human metabolizing enzymes (e.g., CYPs). | Used alongside HLMs to identify which specific enzyme metabolizes a drug candidate [28]. | Allows for isolated study of a single enzyme's activity, clarifying metabolic pathways. |
| Andrastin B | Andrastin B, MF:C28H40O7, MW:488.6 g/mol | Chemical Reagent | Bench Chemicals |
| Goxalapladib | Goxalapladib, CAS:412950-27-7, MF:C40H39F5N4O3, MW:718.8 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Modeling & Simulation Approaches for Interspecies Extrapolation
Population PK (Pop-PK) and Physiologically-Based PK (PBPK) Modeling Fundamentals
In modern drug development, pharmacokinetic (PK) modeling serves as a critical tool for predicting how drugs behave in the body. Among the most advanced approaches are Population PK (Pop-PK) and Physiologically-Based PK (PBPK) modeling, which represent fundamentally different yet complementary methodologies [35]. Pop-PK modeling employs a "top-down" empiric approach, analyzing observed clinical concentration data to identify and quantify sources of variability in drug exposure [35] [36]. In contrast, PBPK modeling utilizes a "bottom-up" mechanistic framework, constructing mathematical representations of the body as a network of physiologically defined compartments to predict drug disposition based on drug properties and human biology [37] [38]. These approaches differ in their epistemological foundations, data requirements, and applications across the drug development continuum, yet both aim to optimize dosing strategies and predict drug behavior in diverse populations [36].
Core Principles and Methodological Foundations
Physiologically-Based Pharmacokinetic (PBPK) Modeling
PBPK models represent the body as a network of anatomically realistic compartments corresponding to specific organs and tissues, interconnected by the circulatory system [37] [38]. Each compartment is defined by physiological parameters including tissue volume, blood flow rate, and tissue composition [38]. Drug movement through this system is described using mass-balance differential equations that account for drug-specific properties and physiological processes [37] [38].
The fundamental equation governing drug distribution in a non-eliminating tissue compartment is:
V_T × dC_T/dt = Q_T × C_A - Q_T × C_VT [38]
Where:
V_T= Tissue volumeC_T= Drug concentration in the tissueQ_T= Blood flow to the tissueC_A= Drug concentration in arterial bloodC_VT= Drug concentration in venous blood leaving the tissue
For eliminating tissues (e.g., liver), an additional term representing metabolic clearance (CL_int × C_VuT) is incorporated into the equation [38]. PBPK models separate system-dependent parameters (species-specific physiology) from drug-dependent parameters (compound-specific properties), enabling predictions across different populations and species [39].
Population Pharmacokinetic (Pop-PK) Modeling
Pop-PK modeling employs nonlinear mixed-effects models to analyze sparse PK data from study populations, identifying and quantifying sources of variability in drug exposure [35] [40]. Unlike PBPK's physiological compartments, Pop-PK compartments are typically empirical without direct physiological correspondence—described as "central" and "peripheral" rather than representing specific organs [35].
The Pop-PK framework estimates:
- Fixed effects: Typical population parameter values (e.g., clearance, volume of distribution)
- Random effects: Inter-individual variability and residual unexplained variability
- Covariate effects: Relationships between patient factors (e.g., age, renal function) and PK parameters [35]
Pop-PK models are developed iteratively, starting with simple structural models and progressively adding complexity to account for covariate relationships that are both statistically significant and biologically plausible [35].
Comparative Analysis: PBPK vs. Pop-PK
Table 1: Fundamental characteristics of PBPK and Pop-PK modeling approaches
| Characteristic | PBPK Modeling | Pop-PK Modeling |
|---|---|---|
| Fundamental Approach | Bottom-up, mechanistic | Top-down, empiric |
| Model Structure | Physiologically defined compartments representing organs/tissues | Empirical compartments (e.g., central, peripheral) |
| Primary Inputs | Drug physicochemical properties, in vitro data, physiological parameters | Observed clinical concentration-time data |
| Variability Assessment | Typically describes average subject; limited inter-individual variability | Estimates inter-individual and residual variability |
| Key Applications | Early development: First-in-human prediction, DDI risk assessment, formulation screening | Late development: Covariate effect quantification, dose optimization in specific populations |
| Regulatory Use | Drug-drug interactions, pediatric extrapolation, biowaivers [41] [38] | Bridging studies, dose justification in special populations, label claims [40] |
| Strengths | Predicts PK before clinical data; simulates tissue concentrations; mechanistic insight | Handles sparse data; quantifies population variability; statistically robust |
| Limitations | Complex parameterization; requires extensive compound data; limited variability assessment | Limited extrapolation capability; requires clinical data; less mechanistic insight |
Table 2: Data requirements and applications across the drug development continuum
| Aspect | PBPK Modeling | Pop-PK Modeling |
|---|---|---|
| Typical Data Requirements | In vitro ADME data, physicochemical properties, enzyme/transporter kinetics [38] | Clinical PK data from studied populations [35] |
| Early Development Applications | Predicting human PK from preclinical data, lead optimization, first-in-human dose selection [38] | Limited application (requires clinical data) |
| Late Development Applications | DDI risk assessment, special population simulations, formulation development [42] [41] | Covariate analysis, dose individualization, exposure-response modeling [40] |
| Special Population Predictions | Pediatric extrapolation, organ impairment, pregnancy [43] [44] [41] | Extrapolation within studied population range [35] |
| Output | Full concentration-time profiles in plasma and tissues | Population parameter estimates and variability |
Experimental Protocols and Workflows
PBPK Model Development Protocol
The development of a robust PBPK model follows a systematic "predict-learn-confirm" cycle [39]:
Step 1: System Data Collection
- Gather physiological parameters for target population (organ weights, blood flows, enzyme abundances)
- Compile demographic information (age, weight, height distributions) [38] [39]
Step 2: Drug Parameter Acquisition
- Determine physicochemical properties (molecular weight, logP, pKa)
- Measure in vitro parameters (plasma protein binding, blood-to-plasma ratio, permeability)
- Quantify metabolic stability (hepatocyte/microsomal clearance, CYP reaction phenotyping)
- Assess transporter affinity where relevant [38]
Step 3: Model Building and Verification
- Implement mathematical structure using specialized software (e.g., GastroPlus, PK-Sim, Simcyp)
- Verify model performance against preclinical PK data in relevant species
- Evaluate predictive accuracy for human PK parameters [38]
Step 4: Model Refinement and Application
- Refine parameters using early clinical data if available ("middle-out" approach)
- Simulate untested scenarios (DDIs, special populations, dosing regimens) [38] [39]
- Conduct sensitivity analysis to identify critical parameters [41]
Pop-PK Model Development Protocol
Pop-PK analysis follows a structured statistical approach to model development:
Step 1: Data Assembly
- Collect all available concentration-time data across studies
- Compile covariate information (demographics, laboratory values, comorbidities)
- Ensure data quality and appropriate assay characterization [35]
Step 2: Base Model Development
- Select structural model (1-, 2-, or 3-compartment)
- Estimate population parameters and variability components
- Assess goodness-of-fit and model stability [35]
Step 3: Covariate Model Building
- Test plausible relationships between covariates and PK parameters
- Use stepwise approaches (forward inclusion/backward elimination)
- Evaluate statistical significance and clinical relevance [35]
Step 4: Model Validation
- Conduct internal validation (bootstrap, visual predictive check)
- Perform external validation if independent dataset available
- Evaluate simulation properties for intended applications [35]
Step 5: Model Application
- Simulate exposure in target populations
- Optimize dosing regimens based on covariate relationships
- Support regulatory submissions and labeling [40]
Research Reagents and Essential Tools
Table 3: Key research reagents and software solutions for PBPK and Pop-PK modeling
| Tool Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| PBPK Software Platforms | PK-Sim, Simcyp, GastroPlus | Implement PBPK model structure and simulations | Whole-body PBPK model development and simulation [38] |
| Pop-PK Software Platforms | NONMEM, Monolix, R/phoenix | Nonlinear mixed-effects modeling | Population PK/PD model development and covariate analysis [35] |
| In Vitro Systems for PBPK | Human liver microsomes, Hepatocytes, Caco-2 cells | Generate drug-specific metabolism and transport parameters | Quantifying intrinsic clearance, permeability, and transporter interactions [38] |
| Analytical Instruments | LC-MS/MS systems | Quantify drug concentrations in biological matrices | Generating PK data for Pop-PK model development [38] |
| Physiological Databases | ICVP, PK-Sim Ontogeny Database | Provide system-specific parameters for PBPK | Incorporating age-dependent physiology and enzyme maturation [44] |
Cross-Species Extrapolation in Comparative Pharmacokinetics
The fundamental differences between PBPK and Pop-PK become particularly significant in cross-species extrapolation, which is essential in translational research. PBPK models excel in this domain because they explicitly incorporate species-specific physiological parameters [44] [38]. By replacing human organ weights, blood flows, and enzyme abundances with corresponding values from preclinical species, PBPK models can predict human PK based on animal data and in vitro information [38]. This capability is particularly valuable for first-in-human dose predictions and estimating clinical starting doses [38].
Pop-PK approaches, while powerful for analyzing human data, have limited application in cross-species prediction due to their empirical nature. However, Pop-PK can be applied within animal species to understand between-animal variability in preclinical models, which can inform human study design [35]. The integration of PBPK predictions followed by Pop-PK analysis of clinical data represents a powerful "learn-and-confirm" paradigm in drug development [43] [39].
For pediatric extrapolation, PBPK models can incorporate ontogeny profiles of drug-metabolizing enzymes and transporters to predict PK across childhood development stages [44]. This approach was successfully demonstrated in the development of moxifloxacin for pediatric populations, where PBPK models informed age-dependent dosing regimens that were subsequently confirmed via Pop-PK analysis of clinical data [43].
Pop-PK and PBPK modeling represent complementary methodologies with distinct strengths and applications in drug development. PBPK's mechanistic, bottom-up approach provides powerful predictive capabilities early in development and enables extrapolation to unstudied populations, including cross-species predictions [38] [39]. Pop-PK's empirical, top-down approach delivers robust quantification of variability and covariate effects in studied populations [35] [40]. The ongoing integration of these approaches—using PBPK for prospective predictions and Pop-PK for analysis of clinical data—represents the state-of-the-art in model-informed drug development, enabling more efficient drug development and optimized dosing strategies across diverse populations [43] [39].
Article | Publish Comparison Guides | Comparative Pharmacokinetics
In the field of drug development, successfully translating pharmacokinetic (PK) data from animal studies to humans is a critical and challenging step. *Allometric scaling provides a empirical yet powerful mathematical framework for this task, enabling the prediction of human PK parameters—such as clearance (CL), volume of distribution (Vss), and half-life (t½)—based on data from preclinical animal species [45] [46]. This methodology is grounded in the principle that many physiological and anatomical processes scale predictably with body size across mammalian species [47] [48]. While its theoretical foundation, particularly the use of a fixed universal exponent, is a subject of ongoing debate [49], allometric scaling remains a cornerstone in drug discovery for making early go/no-go decisions and designing first-in-human (FIH) clinical trials [46] [50]. This guide objectively compares the performance of various allometric scaling methods and alternatives, providing a detailed overview of their principles, applications, and inherent limitations within comparative pharmacokinetics research.
Fundamental Principles of Allometric Scaling
Allometric scaling describes the quantitative relationship between the size of an organism and its biological functions, from whole-body metabolic rate to organ-level physiology.
The Allometric Power Law
The core principle is expressed by the power law equation: Y = a × W^b^, where:
- Y is the biological or pharmacokinetic parameter of interest (e.g., clearance, metabolic rate).
- W is the body weight.
- a is the allometric coefficient, a drug-specific constant.
- b is the allometric exponent, which varies based on the type of parameter [47] [51].
This non-linear relationship explains why a simple mg/kg dose conversion across species is often inaccurate, as it tends to overdose large animals and underdose small ones [47].
Theoretical and Empirical Origins
The practice originates from ecology and the study of metabolic rates. A key empirical observation, *Kleiber's law, established that the basal metabolic rate (BMR) scales with body weight to the power of 0.75 (W^0.75^) [49] [48]. The influential *West, Brown, and Enquist (WBE) framework proposed a theoretical explanation for this 0.75 exponent, based on the fractal nature of nutrient supply networks (e.g., circulatory systems) that fill an organism's volume and are constrained by energy minimization principles [49]. In pharmacology, these principles are extrapolated, assuming that drug clearance, which is often limited by blood flow rates linked to metabolic processes, may also scale with an exponent of 0.75 [49] [51].
From Metabolic Rate to Pharmacokinetic Parameters
The extrapolation applies specific exponents to different PK parameters, grounded in physiological principles:
- Clearance (CL): Often scaled with an exponent (b) of 0.75, analogous to metabolic rate and hepatic blood flow [51].
- Volume of Distribution (V): Typically scaled with an exponent (b) of 1.0, assuming it is proportional to body weight and fluid volumes [51].
- Half-life (t½): Scaled with an exponent (b) of 0.25, derived from the relationship t½ = (0.693 × V) / CL [51].
The following diagram illustrates the logical workflow for applying these principles in a pharmacokinetic study.
Methodological Approaches and Comparison
Multiple scaling methods have been developed, ranging from simple empirical approaches to complex mechanistic models. The table below compares their core features, advantages, and limitations.
Table 1: Comparison of Key Allometric Scaling and Alternative Methods
| Method | Core Principle | Data Requirements | Key Advantages | Primary Limitations & Accuracy |
|---|---|---|---|---|
| Simple Allometry [47] [50] | Direct application of power law (Y = aW^b^) to animal PK data. | Body weight and PK parameters from ≥ 3 animal species. | Simple, fast, inexpensive; useful for early go/no-go decisions [50]. | Less accurate for drugs with significant species-specific metabolism. Fold error: ~2.0-2.25 for human CL and V~ss~ prediction [50]. |
| Fixed Exponent Scaling [51] | Uses pre-defined exponents (e.g., CL=0.75, V=1.0). | Body weight and PK parameters from a single species (often rat). | Extremely simple; allows rapid initial estimates. | Assumes universality, which is often invalid [49]. Accuracy is highly variable and drug-dependent. |
| In Vitro-In Vivo Extrapolation (IVIVE) [46] | Integrates in vitro data (e.g., metabolism, protein binding) with allometry. | Animal PK data + in vitro data (e.g., hepatocyte clearance, f~u~). | Incorporates drug-specific properties; can improve prediction for metabolized drugs. | More complex than simple allometry; requires quality in vitro data. |
| Physiologically-Based Pharmacokinetic (PBPK) Modeling [46] [51] | Mechanistic model simulating drug disposition based on human physiology and drug properties. | Extensive data on system-specific physiology, drug physicochemical properties, and in vitro ADME. | Most accurate and robust; can simulate various scenarios and populations. | Resource-intensive; requires very rich data input and expertise [46]. |
Applications in Drug Development and Research
Allometric scaling is a versatile tool applied across the drug development pipeline, from discovery to clinical dose selection.
- First-in-Human (FIH) Dose Selection: A primary application is predicting a safe Maximum Recommended Starting Dose (MRSD) for clinical trials. This often involves calculating a Human Equivalent Dose (HED) from animal toxicology studies, such as the No-Observed-Adverse-Effect-Level (NOAEL), corrected for body surface area using factors (K~m~) [52] [46]. This approach is recommended by regulatory bodies like the FDA.
- Interspecies Pharmacokinetic Prediction: As demonstrated in Table 1, simple allometry can predict human clearance and volume of distribution from rat data with reasonable accuracy for a wide range of drugs, facilitating early candidate selection [50].
- Extrapolation to Special Populations: Allometric principles are used to scale drug doses from adults to pediatric populations across different ages and body weights, and to adjust for body size in obese patients [49] [53]. However, this requires careful consideration of ontogeny and maturation of drug-metabolizing enzymes in children [53].
- Veterinary Medicine and Zoo Pharmacology: The technique is crucial for determining appropriate drug doses for a wide variety of animal species, from pets to wildlife, where specific PK data is often lacking [45] [47].
Examination of Limitations and Inherent Challenges
Despite its utility, allometric scaling is not a universal law and has several well-documented limitations that researchers must consider.
- The Debate on a Universal Exponent: A significant body of evidence challenges the existence of a single, universal allometric exponent. The 0.75 exponent, while commonly used, is not always accurate, as the true exponent varies based on drug-specific properties and the physiological variables underlying clearance [49]. A critical review suggests moving from a search for a universal "Newtonian" law to a "Darwinian" approach that embraces and explains variability [49].
- Impact of Species-Specific Differences: Scaling accuracy can be poor for drugs affected by factors that are not similar across species. These include [47]:
- Differences in Drug Metabolism: Variations in enzyme expression, function, and metabolic pathways (e.g., dogs lack acetylation metabolism).
- Protein Binding: Differences in plasma protein affinity and capacity.
- Active Transporters: Species differences in the expression and function of uptake/efflux transporters in tissues like the liver and kidney.
- Route of Elimination: Drugs with significant biliary excretion (especially those with molecular weight >350) often deviate from predictions [47].
- Limited Predictive Power for Certain Drugs: Simple allometry often fails for drugs that are highly protein-bound, undergo extensive metabolism with major species differences, or are substrates for active renal secretion [47].
Experimental Protocols and Validation
To ensure reliable results, allometric scaling must be applied using a standardized methodology and validated with experimental data.
Detailed Protocol for Simple Allometry
The following workflow, derived from established practices, outlines the key steps for predicting human pharmacokinetic parameters [47] [51] [50]:
- Data Collection: Gather pharmacokinetic parameters (e.g., Clearance - CL, Volume of distribution at steady state - V~ss~, Half-life - t~½~) from in vivo studies in at least three animal species (e.g., rat, dog, monkey) that span a wide body weight range.
- Logarithmic Transformation: Convert the values of the PK parameter (Y) and the corresponding body weights (W) of each species into logarithmic values (base 10).
- Linear Regression Analysis: Perform a linear regression of log Y against log W using statistical software. The equation of the line is: log Y = b log W + log a.
- Determine Allometric Coefficients: From the regression:
- The slope of the line is the allometric exponent (b).
- The anti-logarithm of the y-intercept is the allometric coefficient (a).
- Predict Human Parameters: Substitute the estimated human body weight (e.g., 70 kg) into the power equation Y = a × W^b^ to predict the human PK parameter.
- Model Validation: Quantify prediction accuracy by comparing extrapolated values with observed human data, often expressed as Mean Error (ME %): ME = [(Extrapolated Value - Observed Value) / Observed Value] × 100 [47].
Case Study: Propofol and Nanochelators
- Propofol Cross-Species Scaling: A study scaling propofol PK from rats to children and adults demonstrated strong allometric relationships. The exponents for clearance (0.78), volume (0.98), and other parameters aligned closely with theoretical values, and model predictions adequately described concentrations in critically ill patients [51].
- Nanochelator Pharmacokinetics: Allometric scaling was successfully applied to predict the PK of a novel deferoxamine nanochelator (DFO-NP) in mice and humans based on rat data. The study used specific exponents (0.75 for clearance, 1 for volumes) and validated the predictions against experimental mouse data, supporting its clinical translatability [54].
Table 2: Key Research Reagent Solutions for Allometric Scaling Studies
| Category | Essential Material / Reagent | Critical Function in Experimentation |
|---|---|---|
| In Vivo Models | Preclinical Species (e.g., Mouse, Rat, Dog, Monkey) | Provides the core pharmacokinetic data (CL, V~ss~, t~½~) from which human parameters are extrapolated. |
| Bioanalytical Tools | HPLC Systems with UV/Fluorescence/ Mass Spectrometry Detection | Used to quantify drug concentrations in biological matrices (e.g., plasma, blood) from animal and human studies. |
| Software & Computation | PK/PD Modeling Software (e.g., Phoenix WinNonlin, NONMEM) | Facilitates regression analysis, model fitting, parameter estimation, and simulation of concentration-time profiles. |
| In Vitro Systems | Hepatocytes, Microsomes, Plasma Protein Binding Assays | Provides data on drug metabolism and protein binding for IVIVE and PBPK approaches, improving prediction accuracy. |
The following graph visualizes the decision-making framework a scientist might use to select the most appropriate scaling method based on the available data and project goals.
Allometric scaling is an indispensable, though imperfect, tool in the toolkit of comparative pharmacokinetists and drug developers. Its power lies in providing rapid, data-driven initial estimates of human pharmacokinetics and safe starting doses, thereby de-risking the early stages of clinical development [45] [46]. However, the field is moving beyond the assumption of a universal scaling law. The future of accurate interspecies extrapolation lies in a more nuanced approach that integrates the principles of allometry with drug-specific properties (e.g., elimination route, protein binding) and patient-specific factors (e.g., age, organ function) [49] [53]. While sophisticated methods like PBPK modeling represent the gold standard for accuracy, simple allometric methods retain significant value for making early, strategic decisions in drug discovery and development.
Model-Informed Precision Dosing (MIPD) in Oncology and CNS Disorders
Model-Informed Precision Dosing (MIPD) represents a paradigm shift in pharmacotherapy, moving away from the traditional "one-dose-fits-all" approach toward personalized dosing strategies that optimize drug exposure for individual patients. This advanced quantitative framework integrates mathematical models of drug pharmacokinetics (PK) and pharmacodynamics (PD) with individual patient demographic and clinical characteristics to support individualized dosage optimization [55]. In essence, MIPD leverages prior knowledge embedded in population pharmacokinetic (popPK) models to inform dosing decisions, with the goal of achieving predefined drug exposure targets associated with desirable clinical outcomes while minimizing adverse effects [56] [57].
The fundamental principle underlying MIPD is the recognition that standard label-recommended dosing regimens may not be effective and safe in all patients due to substantial interpatient variability in drug exposure and response. This variability is particularly problematic for drugs with narrow therapeutic indices, where small deviations from target exposure can lead to therapeutic failure or toxicity [57]. MIPD is especially valuable in clinical contexts characterized by significant inter-individual variability in drug exposure with limited intra-individual variability, and when well-established therapeutic windows predictive of efficacy and safety have been defined [58].
MIPD can be implemented through two primary approaches: a priori dosing and a posteriori dosing. A priori MIPD provides dose recommendations prior to treatment initiation based on patient characteristics (covariates) known to affect PK parameters, utilizing population-based estimations. In contrast, a posteriori MIPD generates dose recommendations during treatment based on therapeutic drug monitoring (TDM) samples, which inform the model about individual PK parameters such as clearance, resulting in more precise, personalized dosing recommendations [58] [56]. Bayesian methods play a crucial role in MIPD implementation, as they enable the adjustment and refinement of population model predictions using observed patient data (e.g., measured drug levels), creating a feedback loop that continuously optimizes dosing based on individual patient response [56].
Fundamental Principles and Methodologies of MIPD
Core Components of MIPD
MIPD integrates several core components to achieve its precision dosing objectives. At the foundation are population pharmacokinetic (popPK) models, which identify factors influencing pharmacokinetic variability and quantify their impact [59]. These models are developed using pharmacokinetic data from patient populations and capture drug-specific parameters such as clearance and volume of distribution, while also quantifying variability between subjects through the incorporation of patient characteristics as covariates [58].
Compared to traditional pharmacokinetic approaches that typically require dense data collection (≥6 samples per participant) under strict controlled conditions, popPK models can handle sparse data (each participant providing only one to a few samples) from patients closer to real-world treatment populations. This not only reduces analysis costs but also provides more accurate estimates of between-subject variability in clinical practice [59].
Bayesian forecasting serves as the computational engine of MIPD, enabling the continuous refinement of model predictions using observed patient data. This approach begins with a "prior" model (typically a population PK model) representing expected outcomes based on patient covariates. As new information becomes available (e.g., therapeutic drug monitoring samples), the model updates its "priors" to generate "posterior" predictions that are better tailored to the individual patient [56]. A key advantage of Bayesian MIPD is its ability to forecast drug exposure for future doses by incorporating updated covariates, unlike alternative methods that assume patient stability and require repeated monitoring when conditions change [56].
Table 1: Core Components of Model-Informed Precision Dosing
| Component | Function | Implementation in MIPD |
|---|---|---|
| Population PK Models | Quantify typical PK parameters and variability between subjects | Identify covariates affecting drug exposure; provide baseline parameter estimates |
| Bayesian Forecasting | Adjust population predictions using individual patient data | Update prior estimates with TDM samples to generate patient-specific posterior parameter estimates |
| Therapeutic Drug Monitoring | Provide individual drug concentration measurements | Serve as observed data to refine model predictions and validate target attainment |
| Clinical Decision Support | Translate model outputs into actionable dosing recommendations | User-friendly software interfaces that integrate patient data and generate optimized dosing regimens |
Technical Workflow of MIPD Implementation
The technical implementation of MIPD follows a structured workflow that transforms patient data into optimized dosing recommendations. This process can be visualized through the following workflow diagram:
Diagram 1: MIPD Technical Workflow showing the integration of patient data with population models through Bayesian estimation to generate optimized dosing recommendations.
Experimental Protocols for MIPD Development and Validation
The development and validation of MIPD approaches follow rigorous methodological protocols that ensure their reliability and clinical applicability. For MIPD tool development, the process typically begins with population pharmacokinetic model development using nonlinear mixed-effects modeling approaches such as NONMEM [59] [60]. This involves collecting rich or sparse pharmacokinetic samples from a representative patient population, with each participant typically providing one to several blood samples at variable times after dose administration [59]. The structural model (e.g., one-compartment or two-compartment) is identified, followed by estimation of between-subject variability and incorporation of patient covariates (demographics, organ function, genetics) that explain variability in PK parameters [60].
Model evaluation employs multiple techniques including goodness-of-fit diagnostics, visual predictive checks, and bootstrap procedures to ensure model robustness and predictive performance [60]. For models intended for MIPD application, external validation in independent patient cohorts is essential to verify predictive performance in real-world clinical settings [58].
When implementing MIPD in clinical practice, the prospective validation protocol typically involves a structured approach. This includes identifying patients requiring the target drug, collecting baseline covariates, obtaining initial drug concentrations (TDM samples), and inputting these data into the MIPD software. The software then generates individualized dosing recommendations based on Bayesian forecasting, which are implemented clinically. Subsequent TDM samples are collected to assess target attainment and refine dosing further [60] [57]. The performance of MIPD is evaluated by comparing key endpoints such as probability of target attainment (PTA), time to target concentration achievement, and distance from target exposure between MIPD-guided dosing and standard dosing approaches [60].
For continual model refinement in clinical practice, a sequential hierarchical Bayesian framework can be implemented. This approach separates the update of individual patient parameters from updating population parameters, enabling continued learning across hospitals or study centers while maintaining data privacy by sharing only summary patient data on the level of model parameters [61].
MIPD Applications in Oncology
Current State of MIPD in Oncology Therapeutics
Oncology represents a particularly promising area for MIPD implementation due to the narrow therapeutic indices, significant interindividual variability, and well-established exposure-response relationships for many antineoplastic agents [58]. The quest to apply MIPD to oncology drugs has gained significant momentum in recent years, reflecting its potential to revolutionize patient care by tailoring treatments to individual pharmacokinetic profiles. However, despite this progress, MIPD has not yet become widely integrated into routine clinical care in oncology [58].
A comprehensive review identified 16 different oncology drugs for which prospective MIPD validation or implementation has been studied [58]. These investigations have primarily focused on attaining adequate drug exposures and reducing inter-individual variability, with demonstrated improvements in clinical outcomes reported for specific agents. For busulfan and high-dose methotrexate, MIPD implementation has shown improved clinical outcomes, while significant reductions in toxicities have been documented for busulfan and cyclophosphamide treatment [58].
The implementation of MIPD in oncology addresses fundamental limitations of traditional dosing approaches. Standard doses for antineoplastic therapies are traditionally determined in phase I trials, often selecting the maximum tolerated dose for further study. This "one-dose-fits-all" approach inherently produces suboptimal outcomes, particularly when significant inter-individual variability in drug exposure combines with well-established exposure-outcome relationships [58]. MIPD offers a more sophisticated approach to individualization that can reduce toxicities, improve quality of life, and in some cases enhance overall survival.
Key Applications and Evidence in Oncology Drugs
Platinum-based antineoplastics represent one of the earliest and most established applications of MIPD in oncology. The Calvert formula for carboplatin dosing, dating back to 1989, represents a pioneering example of MIPD implementation [58]. Carboplatin exhibits a well-defined exposure-toxicity relationship, with increasing area under the curve (AUC) values correlating with higher rates of severe thrombocytopenia. The Calvert formula calculates carboplatin dose based on target AUC and glomerular filtration rate (GFR), recognizing that renal function serves as the principal determinant of carboplatin clearance: Carboplatin dose (mg) = Target AUC (mg/mL·min) × (GFR (mL/min) + 25) [58].
For cisplatin, MIPD has been shown to improve attainment of target exposure, primarily by decreasing subsequent doses as cisplatin clearance decreases over time, most probably due to renal toxicity [58]. Research has demonstrated that cycle count serves as a more influential covariate compared to body surface area (BSA) for cisplatin dosing, highlighting the value of model-informed approaches over traditional covariate-based dosing [58].
Busulfan represents a success story for MIPD in oncology, with prospective studies demonstrating both improved clinical outcomes and reduced toxicity. MIPD of busulfan has been associated with decreased incidence of veno-occlusive disease, a serious complication of high-dose busulfan therapy [56]. Similarly, for high-dose methotrexate, MIPD implementation has shown improved clinical outcomes, though the specific outcomes were not detailed in the available literature [58].
Tyrosine kinase inhibitors (TKIs) represent another drug class benefiting from MIPD approaches. Routine therapeutic drug monitoring of TKIs such as erlotinib, imatinib, lapatinib, and sorafenib has demonstrated high inter- and intra-individual variability in pharmacokinetic behavior. MIPD approaches have proven valuable for optimizing doses, assessing adherence, and evaluating interactions with food and other drugs [55].
Table 2: MIPD Applications in Selected Oncology Drugs
| Drug | Therapeutic Context | MIPD Approach | Demonstrated Benefits |
|---|---|---|---|
| Carboplatin | Various cancers | Calvert formula: Dose = AUC × (GFR + 25) | Improved exposure prediction; reduced thrombocytopenia risk |
| Busulfan | Hematopoietic cell transplantation | Bayesian forecasting with TDM | Reduced veno-occlusive disease; improved clinical outcomes |
| High-dose Methotrexate | Various cancers | Population PK model with TDM | Improved clinical outcomes |
| Cyclophosphamide | Various cancers | Model-informed dosing | Reduced toxicities |
| Tyrosine Kinase Inhibitors (erlotinib, imatinib, etc.) | Various cancers | Therapeutic drug monitoring with popPK models | Optimized dosing; assessment of adherence and drug interactions |
MIPD Implementation Framework in Oncology
The implementation of MIPD for oncology drugs follows a structured framework that can be visualized through the following workflow:
Diagram 2: Oncology MIPD Framework illustrating the integration of patient-specific factors with exposure-response relationships to optimize dosing and clinical outcomes.
MIPD Applications in Central Nervous System (CNS) Disorders
Current Landscape of MIPD in CNS Therapeutics
While the search results provide more limited specific information about MIPD applications in CNS disorders compared to oncology, available evidence indicates that the principles of model-informed precision dosing are similarly applicable to CNS therapeutics. CNS drugs often exhibit complex pharmacokinetic profiles and significant interindividual variability, making them strong candidates for MIPD approaches.
The blood-brain barrier presents a unique challenge for CNS drugs, creating a distinct compartment that must be considered in pharmacokinetic modeling. Additionally, target site drug concentrations in the brain may not directly correlate with plasma concentrations, necessitating sophisticated modeling approaches to bridge this gap. MIPD strategies for CNS drugs must account for these unique distribution characteristics while optimizing dosing regimens to achieve therapeutic concentrations at the site of action.
Several studies referenced in the search results mention CNS applications of MIPD, particularly for antiepileptic drugs and antipsychotic medications [55]. These drug classes typically exhibit narrow therapeutic indices and significant interpatient variability, creating clinical scenarios where MIPD can provide substantial benefit over standard dosing approaches.
Key Applications and Evidence in CNS Drugs
Antiepileptic drugs represent a well-established area for MIPD application in CNS disorders. For levetiracetam, population pharmacokinetic studies in critically ill patients with normal or augmented renal function have enabled the development of specific dosing schemes tailored to this population [55]. Similarly, for valproic acid, population PK models have demonstrated good predictability based on characterization of apparent clearance in pediatric and adult Caucasian patients. These models have identified the influence of co-administered medications (carbamazepine, phenytoin, and phenobarbital) on valproic acid pharmacokinetics, enabling more precise dosing when these common drug combinations are used [55].
Antipsychotic medications constitute another significant application area for MIPD in CNS disorders. Research on long-acting injectable (LAI) atypical antipsychotics including risperidone, paliperidone, and aripiprazole has revealed important pharmacokinetic and pharmacogenetic considerations for optimized dosing. For LAI aripiprazole, CYP2D6 metabolism plays a crucial role in pharmacokinetics, while common factors influencing all these agents include body weight, administration site, and needle characteristics [55]. Evidence suggests that combining pharmacogenetics with pharmacokinetic modeling leads to more effective individualized dosing in antipsychotic therapy [55].
A two-compartmental population PK model of donepezil administered via transdermal patches has enabled characterization of this administration route compared to oral administration, establishing dose equivalence between both routes [55]. This application demonstrates how MIPD can facilitate optimized dosing across different formulation strategies, particularly important for drugs used in chronic CNS conditions like Alzheimer's disease.
Monoclonal antibodies for neuroinflammatory conditions represent an emerging application for MIPD in CNS disorders. While the search results specifically mention infliximab and adalimumab for inflammatory bowel disease [55], similar principles apply to monoclonal antibodies targeting CNS conditions. These biologic therapies typically exhibit complex pharmacokinetics influenced by target-mediated drug disposition and immunogenicity, creating significant interindividual variability that can be addressed through MIPD approaches.
Table 3: MIPD Applications in Selected CNS Disorders
| Drug Category | Specific Agents | MIPD Approach | Key Considerations |
|---|---|---|---|
| Antiepileptic Drugs | Levetiracetam, Valproic acid | Population PK models with renal function and drug interactions | Renal function; metabolic interactions; protein binding |
| Antipsychotics | Risperidone, Paliperidone, Aripiprazole | PK models with pharmacogenetics (CYP2D6) and administration factors | CYP2D6 metabolism; injection site; needle characteristics |
| Alzheimer's Treatments | Donepezil | Transdermal vs. oral route equivalence modeling | Formulation differences; absorption characteristics |
| Monoclonal Antibodies | Anti-TNF agents, others | PopPK models with target-mediated disposition | Immunogenicity; target-mediated clearance; disease burden |
Comparative Analysis: MIPD in Oncology versus CNS Disorders
Methodological Comparisons Across Therapeutic Areas
While MIPD applications in oncology and CNS disorders share fundamental methodological principles, they also exhibit distinct characteristics reflective of their different therapeutic contexts. The comparison below highlights key similarities and differences in MIPD implementation across these two domains:
Diagram 3: Comparative MIPD Focus showing different emphasis in oncology versus CNS disorders, particularly regarding therapeutic priorities and key covariates.
Comparative Data on MIPD Implementation
Table 4: Comparative Analysis of MIPD in Oncology versus CNS Disorders
| Parameter | Oncology Applications | CNS Disorders Applications |
|---|---|---|
| Primary Therapeutic Concern | Balancing efficacy with life-threatening toxicities | Managing chronic conditions with complex efficacy endpoints |
| Key Covariates | Organ function (renal/hepatic), BSA, genetics (DPYD), tumor burden | Blood-brain barrier integrity, CNS penetration, pharmacogenetics (CYP enzymes) |
| Typical PK Sampling | Intensive around chemotherapy cycles; sparse during maintenance | Sparse sampling during chronic therapy; therapeutic drug monitoring |
| Exposure Metrics | AUC, C~max~, time above threshold concentration | Trough concentrations, average steady-state concentration |
| Model Validation Approach | External validation in cancer populations; prospective outcome studies | External validation in psychiatric/neurologic populations; TDM correlation studies |
| Clinical Implementation | Often institutional protocols; specialist-driven | Often outpatient settings; primary care involvement |
| Evidence Level | Prospective studies with clinical outcomes for several drugs | Primarily PK target attainment; limited outcome studies |
Cross-Disciplinary Methodological Considerations
The implementation of MIPD across both oncology and CNS disorders faces several common methodological challenges. Model qualification and validation remains a critical consideration, with optimal strategies for external validation continuing to evolve [58]. The regulatory acceptance of MIPD approaches varies across therapeutic areas and regions, though recent years have seen increasing recognition of model-informed drug development approaches by regulatory agencies [58].
Software implementation represents another shared challenge, with numerous MIPD software tools now available including both commercial offerings (DoseMeRx, InsightRX Nova, MwPharm++, PrecisePK) and non-company platforms (AutoKinetics, BestDose, ID-ODS, NextDose, TDMx, Tucuxi) [57]. The selection of appropriate software tools requires careful consideration of factors including user-friendliness, computational aspects, population model availability, quality validation, and cost [57].
Continued learning approaches represent an emerging methodology relevant to both therapeutic areas. A sequential hierarchical Bayesian framework enables model refinement across patients during clinical implementation, separating the update of individual patient parameters from updating population parameters. This facilitates continued learning across hospitals or study centers while maintaining data privacy through sharing only summary patient data at the model parameter level [61].
The implementation of MIPD relies on sophisticated computational tools and software platforms that enable the complex modeling and simulation tasks required for precision dosing. These resources form the foundation of modern MIPD research and clinical application.
Population PK/PD Modeling Software represents the core computational resource for MIPD development. NONMEM (Nonlinear Mixed Effects Modeling) serves as the industry standard for population pharmacokinetic and pharmacodynamic analysis, providing robust algorithms for parameter estimation in nonlinear mixed-effects models [59]. Complementary tools include R with specialized packages including the Posologyr open-source R package developed for Bayesian individual parameter estimation and dose individualization [55]. Monolix provides an alternative environment for population PK/PD modeling using stochastic approximation expectation maximization (SAEM) algorithms [55].
MIPD Clinical Decision Support Software bridges the gap between complex pharmacometric models and clinical implementation. Currently available platforms include both commercial and academic offerings. DoseMeRx, InsightRX Nova, MwPharm++, and PrecisePK represent commercial platforms offering user-friendly interfaces and technical support [57]. AutoKinetics, BestDose, ID-ODS, NextDose, TDMx, and Tucuxi constitute academic or research-developed platforms with varying features and support structures [57]. These platforms typically provide Bayesian forecasting capabilities, drug-specific modules, and clinical decision support interfaces.
Data Management and Integration Platforms facilitate the handling of complex clinical and pharmacokinetic data. The CONFORM platform by EDETEK offers capabilities to interface with multiple data sources, providing specialized solutions for therapeutic areas including oncology through its ONCO+ accelerator [62] [63]. Such platforms address the critical need for efficient data integration from electronic health records, laboratory systems, and other clinical data sources.
Bioanalytical Technologies form the foundation for generating the high-quality concentration data essential for MIPD. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) represents the gold standard for quantitative determination of most small molecule drugs and metabolites in biological matrices, offering high sensitivity, specificity, and throughput [27]. Immunoassay techniques provide alternative approaches for therapeutic drug monitoring of certain agents, particularly biologics, though with potential limitations in specificity compared to MS-based methods.
Clinical Data Collection Tools support the standardized acquisition of patient covariates and sampling information. Electronic data capture (EDC) systems facilitate structured collection of clinical trial data, while electronic health record (EHR) integration enables extraction of relevant patient characteristics for MIPD in routine care [62]. Specialized forms for documenting precise sampling times and clinical events are essential for minimizing errors in PK data collection.
Biobanking Infrastructure supports the storage and management of biological samples for subsequent analysis. This includes facilities for proper sample processing, storage at appropriate temperatures, and tracking systems to maintain sample chain of custody throughout the analytical process.
Model Qualification and Verification Tools ensure the robustness and reliability of MIPD approaches. Visual predictive checks (VPCs), bootstrap methods, and posterior predictive checks represent standard methodologies for evaluating model performance [60]. External validation datasets from independent patient cohorts provide the most rigorous assessment of model predictive performance in real-world settings [58].
Quality Control Materials support the verification of bioanalytical assay performance over time. These include calibration standards, quality control samples at multiple concentrations, and properly characterized reference standards for drugs and metabolites [27]. Participation in external quality assurance programs provides additional verification of analytical performance.
Standard Operating Procedures (SOPs) document the methodologies for consistent implementation of MIPD in both research and clinical settings. Comprehensive SOPs should cover processes for data collection, sample handling, analytical procedures, model application, and result interpretation to ensure consistency and quality across different providers and settings.
Model-Informed Precision Dosing represents a transformative approach to pharmacotherapy that leverages advanced mathematical modeling to optimize drug exposure for individual patients. The applications of MIPD in both oncology and CNS disorders demonstrate its potential to improve therapeutic outcomes while reducing adverse drug reactions, particularly for agents with narrow therapeutic indices and significant interindividual variability.
In oncology, MIPD has shown promising results for drugs including carboplatin, busulfan, and tyrosine kinase inhibitors, with demonstrated benefits including improved clinical outcomes and reduced toxicities for specific agents [58]. The established exposure-response relationships for many antineoplastic drugs create a strong foundation for further expansion of MIPD approaches in this therapeutic area.
In CNS disorders, MIPD applications for antiepileptic drugs, antipsychotics, and other neuroactive agents address the unique challenges of optimizing therapy for chronic conditions where clinical endpoints may be complex and multifactorial [55]. The blood-brain barrier and target site distribution present special considerations for MIPD in CNS therapeutics that require sophisticated modeling approaches.
The continued advancement of MIPD across therapeutic areas will depend on several key factors, including improved software integration with clinical workflows, standardization of validation approaches, generation of prospective evidence for clinical utility, and implementation of continued learning systems that enable model refinement during clinical use [61] [57]. As these developments progress, MIPD is positioned to become an increasingly integral component of precision medicine, moving beyond traditional "one-size-fits-all" dosing to truly individualized therapeutic optimization.
The comparative analysis presented in this guide provides researchers and clinicians with a framework for understanding both the shared principles and distinctive considerations for MIPD implementation across major therapeutic areas. This foundation supports the rational application and continued development of model-informed approaches to maximize therapeutic benefit while minimizing risk for individual patients.
Posiphen (also known as buntanetap), a small molecule in advanced clinical trials for Alzheimer's and Parkinson's diseases, demonstrates a remarkably consistent metabolic profile across species. This comparative analysis examines Posiphen pharmacokinetics in mouse, rat, dog, and human subjects, revealing similar absorption and metabolism patterns despite physiological differences. The compound shows rapid plasma clearance yet maintains an extended half-life in the brain and cerebrospinal fluid (CSF) across all species studied. Both Posiphen and its primary metabolite N8-norposiphen remain predominant, while the minor metabolite N1-norposiphen—associated with adverse effects—remains a minor constituent, supporting the drug's favorable safety profile. These consistent pharmacokinetic properties provide critical insights for translational research and clinical application in neurodegenerative disorders.
Neurodegenerative diseases represent a significant global health challenge, with Alzheimer's disease alone affecting an estimated 7.1 million Americans and projected to impact 13.9 million by 2060 [64]. Posiphen emerges as a promising therapeutic candidate with a novel mechanism of action, functioning as a translational inhibitor of multiple neurotoxic aggregating proteins (TINAPs) including amyloid precursor protein (APP), tau, α-synuclein, and huntingtin [65] [66]. This multi-target approach positions Posiphen advantageously for treating various neurodegenerative conditions, as many patients present with mixed dementia pathologies [64].
Despite extensive investigation in animal models and human subjects, a comprehensive comparative analysis of Posiphen's pharmacokinetics across species had remained elusive until recently [65] [66] [67]. Understanding interspecies pharmacokinetic consistency is crucial for translational drug development, as it strengthens the predictive value of preclinical models for human clinical outcomes. This case study systematically examines Posiphen's metabolic profile across mouse, rat, dog, and human subjects, with particular emphasis on the implications of its consistent pharmacokinetic properties for therapeutic efficacy, safety, and clinical translation.
Materials and Experimental Methods
Investigational Drug
Posiphen ((3aR)-1, 3a, 8-trimethyl-1, 2, 3, 3a, 8, 8a-hexahydropyrrolo (2, 3-b) indol-5-yl phenylcarbamate tartrate) was manufactured according to Good Manufacturing Practice (GMP) regulations [65] [66]. Standards of deuterated Posiphen and its two primary metabolites (N1- and N8-norposiphen) were synthesized to >99% purity for pharmacokinetic analysis conducted by Charles River Laboratories [65] [66].
Animal Models and Dosing
The animal pharmacokinetic data were compiled from multiple GLP toxicology, biomarker, and efficacy studies [65] [66]. The study included:
- CD-1 mice (n = 7) receiving 65 mg/kg
- Sprague Dawley rats (n = 6) receiving 40 mg/kg
- Beagle dogs (n = 12) receiving 20 mg/kg
Posiphen was administered via capsule to dogs and via gavage to mice and rats, with dose volumes determined according to animal weight on dosing day [65] [66].
Human Participants
Human data were derived from multiple clinical studies:
- Healthy volunteers from single ascending and multiple ascending dose studies
- Alzheimer's and Parkinson's patients from the MCI (NCT01072812), ADCS (NCT02925650), and AD/PD (NCT04524351) studies [65] [66] [68]
Evaluations were based on a sample size of n = 4 for each time point. Posiphen was administered as an immediate-release solid oral dosage form in hard capsule shells manufactured under GMP regulations [65] [66].
Sample Collection and Analysis
Animal samples were collected from plasma, brain tissue, and CSF at multiple time points. Brain samples were homogenized immediately after collection using MeOH/15 mM PBS buffer [65] [66].
Human samples included plasma and lumbar CSF collected via indwelling catheter over 12 hours (at 0, 1, 1.5, 2, 3, 4, 6, 8, and 12 hours) both before and after dosing [65] [66].
Concentrations of Posiphen and its metabolites (N1-norposiphen, N8-norposiphen, and N1,N8-bisnorposiphen) were measured using high-performance liquid chromatography with tandem mass spectrometry (LC-MS/MS) [65] [66]. This validated method achieved a lower limit of quantification (LLOQ) of 0.5 ng/mL for all three analytes in animal studies and 0.100 to 150 ng/mL in human plasma [65] [66].
CYP Reaction Phenotyping
Cytochrome P450 enzyme interactions were characterized through two complementary approaches:
- Microsome incubation: Posiphen was incubated with human liver microsomes with and without isozyme-specific inhibitors, measuring changes in half-life
- Supersome assay: Posiphen was incubated with recombinant CYP isozymes (Supersomes) to identify specific metabolic pathways [65] [66]
CYP induction potential was evaluated using human hepatocyte sandwich-cultures exposed to Posiphen, followed by measurement of CYP isozyme activity and gene expression [65] [66].
Results and Data Analysis
Consistent Metabolic Profiles Across Species
The comparative pharmacokinetic analysis revealed remarkably similar absorption and metabolism patterns of Posiphen across all species tested (mouse, rat, dog, and human) [65] [66] [67]. Population pharmacokinetic analysis demonstrated no significant differences between healthy volunteers, Alzheimer's patients, and Parkinson's patients, indicating that disease state does not alter Posiphen's metabolic handling [65] [66].
The metabolic pathway occurs through demethylation at two primary positions, producing N1-norposiphen and N8-norposiphen metabolites, with further metabolism yielding N1,N8-bisnorposiphen [65] [66]. While all three compounds effectively inhibit neurotoxic proteins, the N1 metabolite has been associated with adverse effects [65] [66] [67].
Comparative Pharmacokinetic Parameters
Table 1: Posiphen Pharmacokinetic Parameters Across Species
| Species | Dose (mg/kg) | Plasma Tâ‚/â‚‚ (h) | Brain/CSF Tâ‚/â‚‚ (h) | Primary Metabolites | Cₘâ‚â‚“ Ratio (Posiphen:N8:N1) |
|---|---|---|---|---|---|
| Mouse | 65 | <8 | >12 | Posiphen, N8 | Similar across species |
| Rat | 40 | <8 | >12 | Posiphen, N8 | Similar across species |
| Dog | 20 | <8 | >12 | Posiphen, N8 | Similar across species |
| Human | 60-80 (total) | <8 | >12 | Posiphen, N8 | Similar across species |
Table 2: Tissue Distribution Characteristics
| Compartment | Clearance Pattern | Half-Life | Clinical Implications |
|---|---|---|---|
| Plasma | Fast clearance | <8 hours | Daily dosing sufficient |
| CSF | Extended presence | >12 hours | Sustained target engagement |
| Brain | Extended presence | >12 hours | Continuous therapeutic effect |
Across all species, Posiphen exhibited rapid clearance from plasma (within 8 hours) but demonstrated an extended half-life exceeding 12 hours in CSF and brain tissue [65] [66] [67]. This differential clearance pattern between peripheral and central compartments has significant therapeutic implications, allowing for sustained target engagement in the nervous system with less frequent dosing.
Metabolic Pathway and Safety Profile
The metabolism of Posiphen occurs primarily through cytochrome P450 enzymes, with consistent patterns observed across species [65] [66]. Critically, N1-norposiphen—the metabolite associated with adverse effects—consistently remained a minor constituent across all species, while Posiphen and N8-norposiphen were the predominant species [65] [66] [67]. This metabolic profile supports Posiphen's favorable safety and tolerability demonstrated in clinical trials [65] [68].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Materials and Methods
| Reagent/Equipment | Function | Application in Posiphen Research |
|---|---|---|
| LC-MS/MS System | Quantification of drug and metabolites | Measurement of Posiphen, N1-, and N8-norposiphen in plasma, CSF, and brain tissue [65] [66] |
| Deuterated Posiphen Standards | Internal standards for accurate quantification | Bioanalytical method validation and sample analysis [65] [66] |
| Human Liver Microsomes | CYP metabolism studies | Reaction phenotyping to identify metabolic enzymes [65] [66] |
| Recombinant CYP Supersomes | Specific CYP isozyme activity | Determination of individual cytochrome P450 contributions to metabolism [65] [66] |
| Human Hepatocyte Sandwich-Cultures | CYP induction studies | Evaluation of Posiphen's potential to induce drug-metabolizing enzymes [65] [66] |
| Kâ‚‚-EDTA Tubes | Plasma sample collection | Anticoagulant treatment for blood samples [65] [66] |
| Dichlorvos Spiking Solution | Stabilization of samples | Prevention of analyte degradation in plasma samples [65] [66] |
| Bagremycin A | Bagremycin A | Bagremycin A is a novel antibiotic with activity against Gram-positive bacteria, fungi, and cancer cells. This product is for Research Use Only (RUO). Not for human or veterinary use. |
| Isosilybin B | Isosilybin B, CAS:142796-22-3, MF:C25H22O10, MW:482.4 g/mol | Chemical Reagent |
Discussion
Implications for Translational Research
The consistent pharmacokinetic profile of Posiphen across species represents a significant finding for translational neuroscience and drug development. The similar absorption and metabolism patterns in rodents, canines, and humans strengthen the predictive value of preclinical models for clinical outcomes [65] [66] [67]. This consistency is particularly valuable for neurodegenerative drug development, where species differences often complicate translation.
The differential clearance between plasma and CNS compartments provides optimal pharmacokinetics for neurodegenerative applications: rapid peripheral clearance minimizes systemic exposure, while extended CNS presence enables sustained target engagement [65] [66]. This profile potentially allows for once-daily dosing while maintaining continuous therapeutic effect on neurological targets.
Therapeutic Advantages and Clinical Relevance
Posiphen's multi-target mechanism against several neurotoxic proteins (APP, tau, α-synuclein) positions it advantageously for treating complex neurodegenerative conditions [65] [69]. The growing recognition that mixed dementia (co-existing pathologies) represents the most common form of dementia underscores the therapeutic potential of broad-spectrum approaches like Posiphen [64].
The consistent metabolic profile where the therapeutically active species (Posiphen and N8-norposiphen) predominate over the adverse-effect-associated metabolite (N1-norposiphen) across species provides strong support for its clinical safety [65] [66] [67]. This is particularly important given the heightened sensitivity to safety concerns in chronic neurodegenerative treatments.
Experimental Workflow
This comprehensive cross-species analysis demonstrates that Posiphen exhibits consistent absorption, metabolism, and distribution patterns across mouse, rat, dog, and human subjects. The stability of its metabolic profile—with predominant levels of the parent drug and beneficial N8 metabolite, and minimal levels of the adverse-effect-associated N1 metabolite—supports its favorable safety and tolerability profile. The rapid plasma clearance coupled with extended CNS retention provides optimal pharmacokinetics for neurodegenerative applications. These findings significantly strengthen the translational framework for Posiphen's continued clinical development in Alzheimer's disease, Parkinson's disease, and potentially other neurodegenerative conditions characterized by protein aggregation pathologies.
Integrating PK/PD Relationships for Predicting Efficacy and Toxicity
The integration of Pharmacokinetic (PK) and Pharmacodynamic (PD) relationships is a fundamental discipline in drug development, providing a quantitative framework for predicting a drug's efficacy and toxicity. PK describes how the body affects a specific drug after administration through the processes of absorption, distribution, metabolism, and excretion (ADME). In contrast, PD measures the drug's biochemical and physiological effects on the body [27]. In the context of comparative pharmacokinetics across species, understanding these relationships is critical for translational research, bridging findings from nonclinical animal models to human clinical trials. The core principle is that a drug's dynamic effects are a function of its concentration at the site of action, which in turn is determined by its PK profile [70].
The combined PK/PD analysis relates drug exposure to the intensity of its therapeutic and adverse effects, enabling the definition of a therapeutic window—the range between the minimum effective concentration (MEC) and the maximum tolerated concentration (MTC) [70]. This approach is particularly valuable for identifying and quantifying sources of interindividual variability (IIV) in drug response, which can be substantial across different species and patient populations due to factors such as age, genetics, disease state, and organ function [71]. For corticosteroids, for instance, substantial IIV in PK has been described, linked to sex- and race-related differences, concomitant medication, and genetic polymorphisms [71].
Foundational PK/PD Concepts and Parameters
Core Pharmacokinetic (PK) Parameters
PK analysis quantifies the journey of a drug through the body. Key parameters are derived from time-concentration curves obtained from preclinical and clinical studies [70].
- Cmax: The maximum concentration of a drug in the bloodstream.
- Tmax: The time at which Cmax is reached.
- AUC (Area Under the Curve): The integral of the concentration-time curve, representing total drug exposure over time.
- Half-life (T½): The time required for the drug concentration to reduce by half, calculated as T½ = (0.693 * Volume of Distribution) / Clearance [70].
- Clearance: The volume of plasma cleared of the drug per unit time.
- Volume of Distribution: A theoretical volume that relates the amount of drug in the body to its concentration in plasma.
Core Pharmacodynamic (PD) and Toxicity Parameters
PD analysis measures the consequences of PK exposure.
- EC50: The drug concentration that produces 50% of the maximum possible therapeutic effect.
- CE50: The drug concentration that produces 50% of a maximum biological effect (e.g., cortisol suppression) [71].
- Minimum Effective Concentration (MEC): The lowest drug concentration needed to produce the desired therapeutic effect.
- Maximum Tolerated Concentration (MTC): The drug concentration above which adverse effects become unacceptable [70].
- Therapeutic Index: A quantitative measure of the relative safety of a drug, often calculated as the ratio of MTC to MEC or the ratio of the AUC for toxicity to the AUC for efficacy.
Methodologies for PK/PD Analysis
A robust PK/PD analysis follows a systematic protocol to collect, model, and interpret data.
Data Collection and Preprocessing
The first phase involves gathering high-quality data from nonclinical and clinical studies [70].
- Obtain PK Data: Collect serial blood samples following drug administration in animal models (e.g., rodents, non-rodents) and human subjects (Phase I trials) to measure drug concentrations over time. This data provides the ADME profile.
- Gather PD Data: In parallel, collect data on the drug's biological effects. This can range from in vitro receptor binding assays and biomarker measurements (e.g., lymphocyte counts, cortisol levels) to clinical outcomes from trials, such as disease activity scores [71] [70].
- Integrate Safety Data: Cross-reference the PK and PD data with safety and toxicity findings from toxicokinetic studies and clinical trials [27].
PK/PD Modeling and Analysis Workflow
The collected data is then synthesized using modeling techniques to define exposure-response relationships.
Diagram 1: PK/PD Modeling and Analysis Workflow
Cross-Species Scaling
A critical step in translational drug development is the extrapolation of PK and PD parameters from animals to humans. This often involves allometric scaling, which uses physiological parameters (e.g., body weight, organ size) to scale doses between species [27]. Furthermore, in vitro PD data, such as the CE50 for lymphocyte suppression or cortisol suppression, can be combined with in vivo PK predictions to anticipate effective dosing regimens in humans [71].
Comparative Analysis: Corticosteroids as a Case Study
Systemic corticosteroids serve as an excellent case study for integrating PK/PD to predict efficacy and toxicity across species. A 2024 systematic review of PK/PD studies in autoimmune and inflammatory diseases highlights the current evidence and gaps [71].
Comparative PK Parameters of Select Corticosteroids
Table 1: Pharmacokinetic Parameters of Corticosteroids Across Species [71]
| Corticosteroid | Bioavailability (%) | Volume of Distribution (L/kg) | Elimination Half-Life | Biological Half-Life | Key Metabolic Pathway |
|---|---|---|---|---|---|
| Prednisone/Prednisolone | 80-100% | 1-2 (Total)4-5 (Unbound) | 2-3 hours | 18-36 hours | Hepatic (CYP) |
| Methylprednisolone | 80-100% | 1-2 | 2-3 hours | 18-36 hours | Hepatic (CYP) |
| Dexamethasone | 60-90% | ~0.5 | ~4 hours | ~54 hours | Hepatic (CYP) |
| Budesonide | ~10% | 1-2 | 2-3 hours | N/R | CYP3A, P-gp Efflux |
N/R = Not Reported in the source material.
Comparative PD and Toxicity Relationships
Table 2: Pharmacodynamic Relationships and Toxicity Correlations of Corticosteroids [71]
| Corticosteroid | Efficacy / PD Relationship | Toxicity / PD Relationship | CE50 (Lymphocyte Suppression) | CE50 (Cortisol Suppression) |
|---|---|---|---|---|
| Prednisolone | Inconclusive/Limited evidence for efficacy PK/PD in autoimmune diseases. | Evidence for relationship between PK and severity of Cushingoid features. | 125 µg/L (Total)10 µg/L (Unbound) | 10 µg/L (Total)1 µg/L (Unbound) |
| Methylprednisolone | Relationship between in vitro lymphocyte sensitivity and clinical response in glomerulosclerosis. | Inverse correlation between AUC and cortisol AUC/suppression ratio. | 10 µg/L | 1 µg/L |
| General Class | Low AUC associated with higher relapse risk (e.g., dexamethasone in ALL). | High/frequent AUC and unbound exposure linked to metabolic, neuropsychiatric, and CV adverse events. | N/A | N/A |
The data reveals substantial interindividual variability (IIV) in corticosteroid PK across species and individuals, influenced by factors such as age, disease state, and genetics [71]. While evidence for a direct PK relationship with clinical efficacy in inflammatory diseases remains limited, the link between drug exposure and toxicity, particularly for prednisolone, is more substantiated. This underscores the critical need for therapeutic drug monitoring and individualized dosing strategies for drugs with a narrow therapeutic window [71] [70].
Successful PK/PD analysis relies on a suite of specialized reagents, tools, and software.
Table 3: Key Research Reagent Solutions for PK/PD Studies [71] [27] [70]
| Item | Function in PK/PD Analysis |
|---|---|
| Validated Bioanalytical Assays (LC-MS/MS) | Precisely quantify drug and metabolite concentrations in complex biological matrices (plasma, tissue) to generate time-concentration data. |
| Biomarker Assay Kits (e.g., ELISA, Multiplex) | Measure PD endpoints such as cytokine levels, receptor occupancy, and physiological biomarkers (e.g., cortisol) to establish the exposure-response relationship. |
| In vitro PD Assay Systems (e.g., Lymphocyte Proliferation) | Assess drug potency (CE50) and mechanism of action in controlled cellular environments, providing initial PD parameters for translation. |
| Stable Isotope-Labeled Drug Standards | Serve as internal standards in mass spectrometry-based assays to improve the accuracy and precision of drug concentration measurements. |
| Allometric Scaling Software | Facilitate the cross-species translation of PK parameters and dose prediction from animal models to humans using physiological data. |
| PK/PD Modeling Software (e.g., NONMEM, Phoenix) | Perform complex population-based modeling and simulation to integrate PK and PD data, identify covariates, and predict outcomes under various scenarios. |
Visualization of Exposure-Response and Therapeutic Window
A central output of PK/PD integration is the visualization of the relationship between drug exposure, efficacy, and toxicity, which defines the therapeutic window.
Diagram 2: PK/PD Relationships Defining the Therapeutic Window
The integration of PK/PD relationships provides a powerful, quantitative approach for predicting the efficacy and toxicity of pharmaceutical compounds. As demonstrated in the corticosteroid case study, this integration is pivotal for understanding interindividual variability and for guiding dose selection across species. Despite the long clinical history of many drugs, the evidence for robust PK/PD relationships in some therapeutic areas remains limited, highlighting a significant opportunity for future research. Prospective studies with well-defined cohorts and advanced modeling techniques are essential to fully quantify these associations. Ultimately, a deep understanding of PK/PD is fundamental for optimizing dosing regimens, improving patient safety, and increasing the success rate of translational drug development.
Addressing Translational Challenges and Optimizing Dosing Strategies
Common Pitfalls in Cross-Species PK Predictions and Their Solutions
Cross-species pharmacokinetic (PK) prediction is a fundamental process in pharmaceutical research and development, aiming to translate drug behavior from preclinical animal models to humans. This translation is essential for determining first-in-human dosing and assessing clinical viability of drug candidates. However, this process is fraught with challenges stemming from physiological, biochemical, and metabolic differences between species. The accuracy of these predictions directly impacts drug development success, yet traditional approaches often fail to adequately account for interspecies variations in key physiological processes.
The process involves sophisticated modeling approaches, including empirical allometric scaling and mechanistic physiologically based pharmacokinetic (PBPK) modeling. These methods attempt to bridge physiological differences between laboratory animals and humans by specifically considering variations in anatomy, physiology, and biochemistry. Research has demonstrated that considering species-specific physiology, plasma protein binding, enzyme and transport kinetics, and tissue-specific gene expression profiles in PBPK modeling significantly increases the accuracy of cross-species extrapolations and thus supports first-in-human trials based on prior preclinical knowledge [72].
Major Pitfalls and Advanced Solutions in PK Predictions
Pitfall 1: Overreliance on Empirical Allometric Scaling Without Mechanistic Basis
Traditional allometric scaling uses simple power laws based on body weight to extrapolate PK parameters from animals to humans. While sometimes effective, this approach often fails to account for species-specific differences in drug metabolism pathways, transporter expression, and tissue binding.
Solution: Implement Mechanistic PBPK Modeling with Species-Specific Physiology Mechanistic PBPK modeling incorporates comprehensive physiological data, including organ sizes, blood flows, and tissue composition, specific to each species. This approach allows for more biologically realistic simulations of drug disposition. A systematic evaluation of different knowledge-driven approaches revealed that successful cross-species extrapolation requires integration of species-specific physiology, plasma protein binding, and enzyme/transporter kinetics [72]. The most accurate extrapolations were achieved when models incorporated both kinetic rate constants and gene expression profiles of relevant enzymes and transporters, demonstrating a synergistic effect on prediction quality.
Table 1: Comparison of Traditional vs. Enhanced Scaling Approaches
| Approach | Methodology | Key Advantages | Limitations |
|---|---|---|---|
| Empirical Allometric Scaling | Uses power laws based on body weight to extrapolate PK parameters | Simple, requires minimal data | Often fails for drugs with species-specific metabolism |
| Mechanistic PBPK Modeling | Incorporates species-specific physiology, tissue composition, and blood flows | Biologically realistic, accounts for metabolic differences | Requires extensive compound-specific and system-specific data |
| PBPK with Gene Expression Data | Adds tissue-specific gene expression profiles of enzymes and transporters | Addresses inter-species differences in expression of key ADME elements | Gene expression may not always correlate directly with functional activity |
Pitfall 2: Neglecting Critical Interspecies Differences in Drug Transport and Excretion
Species variations in transporter expression and function significantly impact drug disposition, particularly for renally excreted drugs and those subject to active transport. These differences often lead to inaccurate predictions of clearance and organ exposure.
Solution: Utilize Advanced In Vitro Transporter Models for Cross-Species Comparison Robust in vitro kidney transporter models like aProximate provide valuable tools for comparing drug handling across species and improving in vitro-in vivo extrapolation. These models use primary isolated kidney proximal tubule cells from multiple species (human, mouse, rat, dog) cultured on Transwell plates to create polarized cell layers that form tight junctions, mimicking the in vivo renal reabsorption and secretion environment [73].
These systems enable direct comparison of apical to basal (Jab) and basal to apical (Jba) flux, net transport measurements, and intracellular drug accumulation across species. For example, studies with para-aminohippurate (PAH) demonstrated net secretion across human, dog, and rat proximal tubule cells, while investigations with the herbicide MCPA revealed species-specific toxicokinetic differences that explained dogs' increased sensitivity compared to humans and rats [73]. This approach helps select the most relevant preclinical species and provides mechanistic insights for regulatory submissions.
Pitfall 3: Inadequate Model Qualification and Validation Methods
Traditional methods for qualifying population PBPK model predictions often fail to account for within-subject correlations and the presence of residual error, leading to overconfident predictions and poor translatability to clinical settings.
Solution: Implement Normalized Prediction Distribution Errors (NPDE) for Robust Model Evaluation NPDE provides a powerful statistical framework for evaluating PBPK model predictions that properly accounts for within-subject correlations and residual error. This method involves computing normalized prediction distribution errors specific to Pop-PBPK models and defines three key measures for evaluating model performance: mean of NPDE, goodness-of-fit plots, and the magnitude of residual error [74].
When applied to a clindamycin PBPK model using prospectively collected plasma concentration data from 29 children, the NPDE-based method qualified the overall model predictions as successful (mean NPDE = 0). However, the approach also revealed potential biases when pediatric subpopulations (e.g., infants) were evaluated separately, demonstrating the method's sensitivity in identifying population-specific prediction failures [74].
Pitfall 4: Failure to Account for Critical Physicochemical Properties in Nanomedicine
Traditional PBPK models for nanoparticles rely on predefined equations and assumptions that fail to fully capture the complexity of biological variability, tumor microenvironments, and organ interactions influenced by nanoparticle physicochemical properties.
Solution: Adopt AI-Powered Multi-View Learning Frameworks Integrating Prior Knowledge A novel multi-view deep learning framework enhances pharmacokinetic predictions for nanoparticles by incorporating prior knowledge of key nanoparticle properties such as size, charge, shape, and surface chemistry into a cross-attention mechanism. This approach enables context-aware feature selection and improves generalization despite small datasets [75].
The model integrates an ensemble learning approach, combining deep learning with XGBoost and Random Forest, significantly outperforming existing AI models in predicting key NP pharmacokinetic parameters (KTRESmax, KTRESn, KTRES50, and KTRESrelease). The interpretability analysis reveals key physicochemical properties driving NP biodistribution, providing biologically meaningful insights rather than functioning as a black box [75].
Table 2: Key Nanoparticle Properties Influencing Pharmacokinetics and Experimental Assessment Methods
| Property | Impact on PK | Experimental Assessment Methods |
|---|---|---|
| Hydrodynamic Diameter | Determines renal clearance, RES uptake, and tissue penetration | Dynamic light scattering |
| Zeta Potential | Influences protein binding, cellular uptake, and circulation time | Electrophoretic light scattering |
| Surface Chemistry | Affects stealth properties, targeting, and immune recognition | Chromatography, spectrometry |
| Shape | Impacts margination, cellular uptake, and clearance pathways | Electron microscopy |
| Core Material | Determines degradation rate, drug release, and toxicity | Material characterization techniques |
Detailed Experimental Protocols for Robust Cross-Species PK
Protocol 1: Comprehensive Cross-Species PK Study Design
The lenvatinib cross-species investigation provides an exemplary protocol for thorough PK characterization [76]. This study evaluated PK in mice, rats, dogs, and monkeys following both intravenous and oral administration to fully characterize disposition across species.
Bioanalytical Method Details: Researchers developed a simple HPLC-UV method validated according to FDA bioanalytical guidelines. The assay quantified lenvatinib at 5–100,000 ng/mL using only 50 μL of plasma, demonstrating exceptional dynamic range. Sample preparation involved liquid-liquid extraction with diethyl ether after adding an internal standard and phosphate buffer (pH 8). Chromatography employed a Mightysil RP-18 GP column with a mobile phase of water containing 50 mM sodium dodecyl sulfate (pH 2.5)/acetonitrile (55.5/45, v/v) at 1.2 mL/min flow rate, detecting at 253 nm [76].
PK Study Design: Animals received lenvatinib intravenously or orally at doses ranging from 3 to 30 mg/kg. The high dose range, much greater than clinical doses, necessitated the wide dynamic range of the bioanalytical method. Researchers collected serial blood samples, processed plasma, and analyzed concentrations using the validated HPLC-UV method. PK parameters including clearance, volume of distribution, and bioavailability were calculated using non-compartmental analysis.
Key Finding: The study successfully predicted human systemic exposure using allometric scaling, demonstrating the utility of comprehensive cross-species PK characterization [76].
Protocol 2: In Vitro Transporter Flux Assay for Renal Excretion Prediction
The aProximate kidney transporter model offers a standardized approach for assessing species differences in renal drug handling [73].
Cell Culture Protocol: Primary isolated kidney proximal tubule cells from human, mouse, rat, and dog are cultured on Transwell plates (24-well for transporter assays, 96-well for toxicity assays). Cells are maintained with specific media formulations and used upon forming confluent, polarized monolayers with tight junctions, typically requiring 3-7 days in culture.
Transport Studies: Compounds are added to either the apical or basolateral compartment, with sampling from the opposite compartment at 0, 30, 60, 90, and 120 minutes. Experiments include assessments with and without specific transporter inhibitors (e.g., probenecid for OAT1) to elucidate mechanisms. Each condition is performed in triplicate using cells from at least three different biological donors per species.
Measurements and Calculations: Researchers measure apical to basal flux (Jab), basal to apical flux (Jba), and calculate net flux (Jnet = Jba - Jab). Additionally, intracellular drug and metabolite concentrations can be determined, providing insights into accumulation and metabolism.
Application: This protocol successfully identified species differences in MCPA handling, explaining dogs' heightened sensitivity and supporting their exclusion as non-relevant models for human risk assessment [73].
Integrated PK Prediction Workflow: This diagram illustrates how combining AI, mechanistic modeling, and traditional approaches enhances prediction accuracy.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Platforms for Cross-Species PK Studies
| Tool/Reagent | Function | Application in Cross-Species PK |
|---|---|---|
| aProximate Primary Kidney Cells | In vitro model of renal proximal tubule transport | Assess species differences in renal secretion/reabsorption [73] |
| Transwell Plates | Support polarized cell culture for transport studies | Measure vectorial transport (apicalbasolateral) [73] |
| PBPK Modeling Software | Simulate ADME processes using physiological parameters | Implement cross-species extrapolation with species-specific parameters [72] |
| Validated Bioanalytical Methods | Quantify drug concentrations in biological matrices | Generate reliable PK data across species [76] |
| NPDE Statistical Package | Evaluate PBPK model performance with proper error accounting | Quality-check cross-species predictions before clinical translation [74] |
| Flavipucine | Flavipucine|Antibacterial Compound|RUO | Flavipucine is a pyridione epoxide with potent research applications in antibacterial and cancer cell studies. For Research Use Only. Not for human use. |
Cross-species PK predictions remain challenging but have seen significant advances through integrated approaches combining sophisticated in vitro models, mechanistic modeling, and emerging AI technologies. The most successful strategies incorporate species-specific physiology, transporter function, and physicochemical properties while implementing robust validation methods like NPDE. Future directions point toward increased integration of AI with PBPK modeling, expanded use of humanized models, and greater incorporation of systems biology data to further enhance prediction accuracy. These advances will ultimately improve the efficiency of drug development and the safety of first-in-human trials.
Strategies for Drugs with Narrow Therapeutic Indices
Narrow Therapeutic Index (NTI) drugs are defined by the U.S. Food and Drug Administration as "those drugs where small differences in dose or blood concentration may lead to serious therapeutic failures and/or adverse drug reactions that are life-threatening or result in persistent or significant disability or incapacity" [77]. The therapeutic index quantitatively represents the margin between a drug's effective concentration and its toxic concentration, calculated as the ratio of the dose that produces a toxic response in 50% of the population (TD50) to the dose that produces a therapeutic response in 50% of the population (ED50) [78]. Drugs with a narrow therapeutic index present unique challenges throughout their development lifecycle, from initial discovery through clinical use, requiring specialized strategies to ensure patient safety while maintaining therapeutic efficacy.
The clinical significance of NTI drugs stems from their steep dose-response relationship, where minimal variations in drug exposure can precipitate serious consequences. For example, the anticoagulant warfarin exemplifies these challenges, as its effective antithrombotic dose overlaps with doses that may cause bleeding complications [78]. As of January 2024, the FDA has identified 33 drug products containing 14 distinct active ingredients as NTI drugs in their respective product-specific guidances for generic drug development [77]. Understanding and managing the risks associated with these pharmaceuticals requires a multifaceted approach encompassing precise dosing, careful therapeutic monitoring, and stringent regulatory oversight.
Regulatory and Bioequivalence Standards
Regulatory Classification Frameworks
Regulatory agencies worldwide have established specialized frameworks for evaluating NTI drugs, with particular emphasis on generic versions. In 2015, the FDA formed the NTI Drug Working Group to develop a consistent approach for identifying NTI drugs and resolving related scientific and regulatory issues transparently [77]. This working group focuses on evaluating potential NTI drugs based on five general characteristics, as exemplified in the case study of theophylline drug products [77]. The regulatory approach has matured from a "one size fits all" standard to product-specific bioequivalence requirements that account for the unique properties of each NTI drug [79].
The classification of a drug as having a narrow therapeutic index carries significant implications for its development pathway and clinical use. Notably, some drugs may exhibit NTI characteristics for one indication but not for others. Aspirin, for instance, demonstrates NTI properties when prescribed for rheumatoid arthritis at doses of 4-6 grams daily, which approach toxicity thresholds, whereas it does not exhibit these characteristics at lower antiplatelet or analgesic doses [80]. This indication-specific variability necessitates careful evaluation throughout the drug development process.
Comparative Bioequivalence Requirements
Regulatory agencies worldwide have established stricter bioequivalence standards for generic NTI drugs compared to conventional medications. The following table summarizes the key bioequivalence criteria across major regulatory authorities:
Table 1: Bioequivalence Criteria for NTI Drugs Across Regulatory Agencies
| Agency | Study Design | Acceptable Confidence Interval Range | Additional Requirements |
|---|---|---|---|
| FDA [80] | 4-way fully replicated crossover | 90% CI must fall within 80.00-125.00% | Must satisfy both reference-scaled average bioequivalence (95% upper confidence bound ≤ 0) and within-subject variability ratio (σWT/σWR ≤ 2.5) |
| EMA [80] | Parallel, crossover | Tightened range of 90.00-111.11% for AUC | For Cmax, either regular range (80.00-125.00%) or tightened range based on safety/efficacy importance |
| Health Canada (TPD) [80] | Parallel, crossover | Tightened range of 90.00-111.11% for AUC | Regular range (80.00-125.00%) for Cmax |
| ANVISA (Brazil) [80] | Parallel, crossover | Regular range of 80.00-125.00% | Based on SmPC recommendations |
| NMPA (China) [80] | Parallel, crossover | Regular range of 80.00-125.00% | Fasting and Fed conditions required |
The FDA's approach is particularly rigorous, requiring a 4-way fully replicated study design regardless of the drug's variability, with mandatory evaluation under both fasting and fed conditions [80]. Generic applicants must demonstrate bioequivalence using both regular average bioequivalence and reference-scaled average bioequivalence approaches simultaneously, ensuring even small variations between products are detected and controlled.
Experimental Strategies for NTI Drug Development
Bioequivalence Study Methodologies
The development of generic NTI drugs requires sophisticated experimental designs to demonstrate therapeutic equivalence. The FDA mandates a 4-way fully replicated crossover design, wherein each participant receives both the test and reference product on two separate occasions [80]. This design enables precise estimation of within-subject variability for both formulations, a critical parameter for NTI drugs where even minor variations can have significant clinical consequences.
The statistical analysis for NTI drugs extends beyond conventional average bioequivalence criteria. Applicants must additionally demonstrate reference-scaled average bioequivalence, where the 95% upper confidence bound for the comparison must be ≤0, and the ratio of within-subject standard deviations between test and reference products must not exceed 2.5 [80]. This multifaceted statistical approach ensures that generic NTI drugs exhibit consistent performance not only in average exposure but also in variability compared to the reference product.
Diagram 1: NTI Drug Bioequivalence Assessment Workflow
Pharmacokinetic and Pharmacodynamic Modeling
Advanced modeling and simulation approaches play a crucial role in NTI drug development. Physiologically Based Pharmacokinetic (PBPK) modeling and Pharmacokinetic/Pharmacodynamic (PK/PD) modeling help characterize the complex relationship between dose, exposure, and response for NTI drugs [79]. These models integrate in vitro data with physiological parameters to predict drug behavior in humans, aiding in dose selection and identifying critical factors that influence drug exposure.
The FDA's regulatory science initiatives have included awarded grants for population pharmacokinetic and pharmacodynamic modeling, dose-toxicity modeling, and simulation for NTI drugs [79]. These research efforts aim to develop more sophisticated methods for characterizing the therapeutic index and predicting clinical performance based on limited data. For instance, research on tacrolimus and levetiracetam has focused on therapeutic index evaluation using modeling approaches [79], while other projects have explored pharmacometric modeling for generic drug substitutability evaluation and post-marketing risk assessment [79].
In Vitro Dissolution and Quality Control
Stringent in vitro dissolution testing represents another critical strategy for ensuring the quality and performance of NTI drug products. Regulatory agencies often require more rigorous dissolution specifications for NTI drugs compared to conventional medications. These specifications typically include:
- Multiple dissolution conditions covering various pH levels to assess robustness
- Closer similarity requirements (f2 values) between test and reference products
- Evaluation of dissolution profiles using model-independent and model-dependent methods
- Testing of multiple lots to establish consistent performance
The product-specific guidances issued by FDA for NTI drugs like tacrolimus, phenytoin, levothyroxine, and carbamazepine include detailed recommendations for in vitro dissolution studies that exceed standard requirements [79]. These enhanced quality controls help ensure consistent in vivo performance by detecting potential formulation differences that might impact drug absorption and exposure.
Species Comparison in Pharmacokinetic Research
Cross-Species Extrapolation Challenges
Comparative pharmacokinetics across species presents particular challenges for NTI drugs, where small differences in metabolic pathways, protein binding, or transporter expression can significantly alter exposure-response relationships. The therapeutic index established in animal models may not directly translate to humans due to species-specific differences in drug disposition and sensitivity [78]. Understanding these interspecies variations is essential for appropriate dose selection during first-in-human studies and for contextualizing toxicity findings from nonclinical studies.
Several factors contribute to discordance in NTI drug behavior across species:
- Differences in metabolic enzyme expression and activity
- Variations in plasma protein binding and tissue distribution
- Species-specific transporter expression and affinity
- Dissimilar drug receptor structure and binding affinity
- Unique physiologic parameters (gastric emptying, blood flow, organ size)
These factors necessitate careful experimental design when extrapolating NTI drug data from animal models to humans, with particular attention to exposure matching rather than simple dose normalization by body weight or surface area.
Allometric Scaling and In Vitro-In Vivo Extrapolation
Allometric scaling approaches combined with in vitro-in vivo extrapolation (IVIVE) represent key methodologies for addressing species differences in NTI drug development. These techniques incorporate physiological parameters across species to predict human pharmacokinetics based on animal data and in vitro systems. The workflow typically involves:
- Determining fundamental pharmacokinetic parameters (clearance, volume of distribution) in multiple animal species
- Measuring in vitro drug metabolism and transport in human and animal-derived systems
- Applying allometric scaling with species-specific correction factors
- Verifying predictions using PBPK modeling platforms
For NTI drugs, the accuracy of these predictions is particularly critical, as small errors in projected human exposure could lead to subtherapeutic or toxic outcomes. The FDA's regulatory science initiatives have supported research in this area, including grants for "Pharmacometric modeling and simulation for a generic drug substitutability evaluation and post marketing risk assessment" [79].
Diagram 2: Cross-Species Pharmacokinetic Strategy for NTI Drugs
Essential Research Reagents and Methodologies
Critical Research Tools for NTI Drug Evaluation
The complex evaluation of NTI drugs requires specialized research reagents and methodologies to accurately characterize their pharmacokinetic and pharmacodynamic properties. The following table outlines essential tools and their applications in NTI drug development:
Table 2: Essential Research Reagents and Methodologies for NTI Drug Development
| Research Tool | Function | Application in NTI Drug Development |
|---|---|---|
| Stable Isotope-Labeled Analytes [79] | Internal standards for bioanalytical assays | Enable precise quantification of drug concentrations in biological matrices for accurate pharmacokinetic profiling |
| Recombinant Drug-Metabolizing Enzymes [79] | In vitro metabolism studies | Identify primary metabolic pathways and potential drug interactions that could alter NTI drug exposure |
| Transporter-Expressing Cell Systems [79] | Transporter interaction assessment | Evaluate potential transporter-mediated drug interactions that may significantly impact NTI drug disposition |
| Human Hepatocytes and Liver Microsomes [79] | Hepatic clearance prediction | Estimate intrinsic clearance and potential for hepatically-mediated drug interactions |
| PBPK Modeling Software [79] | In vitro-in vivo extrapolation | Integrate physicochemical, in vitro, and preclinical data to predict human pharmacokinetics |
| Validated Bioanalytical Assays [80] | Drug concentration quantification | Support bioequivalence studies with precise measurement of drug levels in plasma/serum |
| Clinical PK/PD Modeling Platforms [79] | Exposure-response analysis | Characterize relationship between drug concentrations, therapeutic effects, and adverse reactions |
These research tools enable scientists to address the unique challenges posed by NTI drugs throughout the development process. The precision and accuracy afforded by these methodologies are essential for establishing appropriate dosing regimens and safety margins for drugs with narrow therapeutic windows.
Biomarker and Therapeutic Drug Monitoring Assays
The successful clinical use of NTI drugs often depends on the availability of reliable biomarkers or therapeutic drug monitoring (TDM) assays that can guide dose individualization. For example, warfarin dosing is guided by International Normalized Ratio (INR) monitoring, which provides a quantitative measure of anticoagulant effect that correlates with both efficacy and bleeding risk [80]. The development of such monitoring tools is an integral component of NTI drug strategy, enabling clinicians to maintain patients within the narrow therapeutic window.
Novel biomarker development for NTI drugs represents an active area of research, particularly for drugs where direct concentration monitoring is not feasible or where response lags behind plasma concentrations. Emerging approaches include:
- Pharmacogenetic testing to identify patients with altered drug metabolism
- Biomarkers of pharmacological effect rather than drug concentration
- Point-of-care testing devices for rapid dose adjustment
- Continuous monitoring systems for drugs with rapidly changing concentration-effect relationships
These monitoring strategies are particularly important in the context of interspecies differences, as the relationships between dose, concentration, and effect established in animal models may require verification and refinement in humans based on clinically accessible biomarkers.
Drugs with narrow therapeutic indices present unique challenges throughout the development and clinical use continuum, necessitating specialized strategies to ensure their safe and effective application. The regulatory landscape for these products has evolved to include stricter bioequivalence standards, with requirements for replicated study designs and tightened confidence intervals for generic versions. From a research perspective, sophisticated methodologies including PBPK modeling, advanced dissolution testing, and careful species comparison are essential components of a comprehensive development program for NTI drugs.
The future of NTI drug development will likely involve even more sophisticated approaches to managing their inherent risks. Emerging technologies such as physiologically based pharmacokinetic modeling, microsampling techniques for improved pharmacokinetic characterization, and model-informed drug development represent promising avenues for further enhancing the safety profile of these critical medications. Furthermore, ongoing harmonization efforts between regulatory agencies regarding NTI drug classification and standards may help enhance clarity and consistency during the drug development and regulatory review processes [77]. As these advanced strategies continue to evolve, they promise to improve the therapeutic outlook for patients requiring medications with narrow therapeutic windows.
Optimizing Dosing Regimens Using Steady-State and AUC Simulations
In drug development, steady-state pharmacokinetics and Area Under the Curve (AUC) simulations are fundamental for determining safe and effective dosing regimens. Steady state occurs when the rate of drug administration equals the rate of drug elimination from the body, resulting in consistent drug concentrations within a therapeutic window over time [81] [82]. This dynamic equilibrium is crucial for maintaining therapeutic levels where medication is effective without causing toxicity [83].
The AUC, particularly when measured at steady-state (AUC0-Ï„), serves as a key metric for overall drug exposure [84]. For drugs with constant clearance, the AUC during a steady-state dosing interval is identical to the total AUC from a single dose, enabling researchers to extrapolate exposure data from single-dose studies to predict steady-state conditions [83] [82]. This equivalence facilitates more efficient clinical trial design by potentially eliminating the need for multiple preliminary trials testing different dosing regimens [83].
The time to reach steady-state concentration is governed primarily by a drug's elimination half-life, with approximately five half-lives required to achieve 97% of steady-state levels [82] [84]. This relationship has critical implications for dosing strategy design, particularly for drugs with extended half-lives where therapeutic levels must be achieved rapidly.
Fundamental Principles of Steady-State Pharmacokinetics
Key Parameters and Their Clinical Significance
At steady-state, several pharmacokinetic parameters become particularly important for dosing optimization:
- Average steady-state concentration (Css): The consistent concentration around which drug levels fluctuate during repeated dosing. This can be calculated using the formula: Css = AUC0-Ï„/Ï„, where Ï„ is the dosing interval [82].
- Peak and trough concentrations (Cmax and Cmin): The maximum and minimum drug concentrations during a dosing interval at steady state. These parameters help define the therapeutic window and assess potential toxicity risks [83].
- Accumulation ratio: An index of how much a drug accumulates in the body with repeated dosing compared to a single dose [81].
For drugs administered intravenously, the average steady-state concentration can be directly calculated using the equation: Css = R0/CL, where R0 is the rate of drug input and CL is clearance [82]. This straightforward relationship demonstrates that steady-state levels are proportional to the infusion rate.
Loading Dose Strategy
When the time to reach steady state is therapeutically unacceptable (e.g., for antibiotics in critically ill patients or drugs with long half-lives), a loading dose strategy may be employed. A loading dose is an initial, larger dose designed to rapidly achieve therapeutic concentrations, followed by maintenance doses to sustain steady state [81] [82]. The loading dose can be calculated using the formula:
LD = Css • Vd/F
Where LD is the loading dose, Css is the desired steady-state concentration, Vd is the volume of distribution, and F is bioavailability [81]. This approach allows clinicians to achieve target concentrations quickly without altering the time to reach steady state, which remains dependent on the drug's half-life [84].
Experimental Approaches for AUC and Steady-State Determinations
Cross-Species Pharmacokinetic Study of Lenvatinib
A comprehensive study developed a simple high-performance liquid chromatography with ultraviolet detection (HPLC-UV) method to quantify lenvatinib, a tyrosine kinase inhibitor, across multiple species [85].
Table 1: Bioanalytical Method Validation for Lenvatinib Quantification
| Validation Parameter | Specification | Result |
|---|---|---|
| Quantification Range | 5–100,000 ng/mL | Achieved using 50 μL of plasma |
| Intra-batch Accuracy | Within ±15% RE | Met acceptance criteria |
| Inter-batch Accuracy | Within ±15% RE | Met acceptance criteria |
| Intra-batch Precision | Within 15% RSD | Met acceptance criteria |
| Inter-batch Precision | Within 15% RSD | Met acceptance criteria |
The experimental protocol involved:
- Sample Preparation: Lenvatinib and internal standard (ER-227326) were extracted from 50 μL of plasma using liquid-liquid extraction with diethyl ether after adding 0.1 mol/L phosphate buffer (pH 8) [85].
- Chromatographic Conditions: Separation used a Mightysil RP-18 GP column (4.6 × 250 mm, 5 μm) with a mobile phase of water with 50 mM sodium dodecyl sulfate (pH 2.5)/acetonitrile (55.5/45, v/v) at 1.2 mL/min flow rate [85].
- Detection: Ultraviolet detection at 253 nm [85].
- PK Study Design: Lenvatinib was administered intravenously or orally to mice, rats, dogs, and monkeys to characterize cross-species pharmacokinetics [85].
This robust assay demonstrated that lenvatinib bioavailability was approximately 64–78% across all tested species, with relatively low total clearance and volume of distribution. The study successfully used allometric scaling to predict human systemic exposure, demonstrating the value of cross-species PK characterization [85].
Innovative Vancomycin AUC Estimation Methods
Research on vancomycin dosing optimization proposed two innovative approaches to estimate AUC at steady state (AUCSS) using a two-compartment model and multiple concentration measurements after the first dose [86].
Table 2: Comparison of Vancomycin AUC Estimation Methods
| Method | Samples | Model | AUC0-∞:AUCref Ratio | Bias (%) |
|---|---|---|---|---|
| Method 1 | 4 concentrations (1.5, 2.5, 9.5, 11.5 h) | Two-compartment | 0.98–1.00 | -0.10 to -2.09 |
| Method 2 | 3 concentrations | Two-compartment | 0.96–0.99 | -1.30 to -3.59 |
| Method 3 | 2 concentrations | One-compartment | 0.44–0.69 | -30.75 to -55.53 |
The experimental workflow for Method 1, the most accurate approach, involved:
- Sample Collection: Four blood samples drawn at specific time points after the first vancomycin dose (1.5, 2.5, 9.5, and 11.5 hours) [86].
- Model Application: Using a two-compartment pharmacokinetic model with the equation:
C = R • e-αt' + S • e-βt'
where R and S represent complex combinations of pharmacokinetic parameters [86].
- Parameter Calculation: Determining distribution and elimination rate constants (α and β) from the concentration-time data [86].
- AUC Estimation: Calculating AUC extrapolated to infinity (AUC0-∞) using the derived parameters [86].
This approach achieved significantly better accuracy than traditional one-compartment methods, enabling early achievement of target pharmacokinetic/pharmacodynamic indices by the third or fourth dose rather than waiting until steady state is reached [86].
Diagram 1: Workflow for Steady-State and AUC-Based Dosing Optimization. This diagram illustrates the systematic approach from initial single-dose studies through model development and simulation to clinical verification of optimized dosing regimens.
Cross-Species Comparative Pharmacokinetics
Posiphen Pharmacokinetics Across Species
A comparative analysis of Posiphen, a neuroprotective compound, demonstrated similar absorption and metabolism patterns across mouse, rat, dog, and human subjects [65].
Table 3: Comparative Pharmacokinetics of Posiphen Across Species
| Species | Dose | Matrix | Key Findings |
|---|---|---|---|
| CD-1 Mice | 65 mg/kg | Plasma, CSF, Brain | Fast clearance in plasma (<8 h); extended half-life in CSF/brain (>12 h) |
| Sprague Dawley Rats | 40 mg/kg | Plasma | Fast clearance in plasma (<8 h); similar metabolic profile |
| Beagle Dogs | 20 mg/kg | Plasma | Fast clearance in plasma (<8 h); predominant Posiphen and N8 metabolite |
| Humans | Various | Plasma, CSF | Similar absorption/metabolism across healthy volunteers, Alzheimer's and Parkinson's patients |
The experimental methodology included:
- Sample Collection: Blood samples collected via saphenous vein (mice), other suitable sites (rats, dogs), or indwelling catheter (humans) into K2-EDTA tubes on wet ice [65].
- Sample Processing: Plasma separation by centrifugation (3200× g for 10 min at 4°C) within one hour of collection [65].
- Brain Homogenization: For tissue distribution studies, whole brains were homogenized in MeOH/15 mM PBS (1:2, v:v) at a 1:9 tissue-to-buffer ratio [65].
- Analytical Method: Quantification of Posiphen and metabolites (N1-norposiphen, N8-norposiphen) using validated LC-MS/MS methods with lower limits of quantification of 0.5 ng/mL for all analytes [65].
This comprehensive cross-species comparison demonstrated that Posiphen and its beneficial N8 metabolite were predominant across species, while the potentially adverse N1 metabolite remained a minor constituent, supporting the drug's safety profile [65].
Meropenem Dosing Optimization in Critically Ill Patients
A study on meropenem pharmacokinetics in critically ill patients highlighted the importance of steady-state optimization in special populations, with findings relevant to cross-species extrapolation [87].
The research utilized a two-compartment model with first-order elimination to characterize meropenem's plasma pharmacokinetics. Covariate testing revealed that CKD-EPI estimated glomerular filtration rate (eGFR) and recent surgery significantly affected drug clearance. The relationships were quantified as:
- CL = CLpop × (eGFR/97)0.58
- CLsurgery = CLpop × e0.51
Monte Carlo simulations demonstrated that continuous infusion achieved the highest probability of target attainment (PTA) - 73% of simulated scenarios across various MIC values and renal function levels, compared to 54.4% for extended infusion and 45.1% for intermittent infusion [87]. This approach successfully optimized dosing for both day 1 and steady-state conditions in critically ill patients.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 4: Essential Research Materials for Steady-State and AUC Studies
| Reagent/Material | Specification | Research Function |
|---|---|---|
| HPLC-UV System | Mightysil RP-18 GP column (4.6 × 250 mm, 5 μm) | Drug quantification in biological samples [85] |
| LC-MS/MS System | Validated per FDA guidelines | Sensitive quantification of drugs and metabolites [65] |
| Blank Plasma | Species-specific with sodium heparin | Matrix for calibration standards and quality controls [85] |
| Stable Isotope Standards | Deuterated analogs >99% purity | Internal standards for precise quantification [65] |
| Mobile Phase Additives | 50 mM sodium dodecyl sulfate (pH 2.5) | Chromatographic separation optimization [85] |
| Extraction Solvents | Diethyl ether, methanol, acetonitrile | Sample preparation and analyte extraction [85] |
| Population PK Software | NONMEM (version 7.5) | Pharmacokinetic modeling and simulation [86] |
Diagram 2: Logical Relationships in Dosing Optimization. This diagram shows the conceptual flow from fundamental pharmacokinetic principles through modeling and simulation to the ultimate goal of optimized dosing regimens.
Steady-state pharmacokinetics and AUC simulations provide powerful frameworks for optimizing dosing regimens across the drug development pipeline. The integration of robust bioanalytical methods, physiologically-relevant pharmacokinetic modeling, and cross-species extrapolation enables researchers to design dosing strategies that maximize therapeutic efficacy while minimizing adverse effects. As demonstrated in the case studies presented, these approaches successfully bridge from preclinical species to human applications, supporting the development of personalized medicine strategies that account for inter-individual and inter-species variability in drug disposition.
Selecting the optimal dosing regimen is a critical decision in drug development, balancing therapeutic efficacy, safety, and patient compliance. The choice between a once-daily (QD) and twice-daily (BID) schedule is far from trivial; it fundamentally influences a drug's clinical effectiveness and commercial viability. This case study examines how Pharmacokinetic (PK) modeling and simulation provide a powerful, data-driven framework to resolve this dilemma, moving beyond assumptions to quantitatively predict a drug's behavior under different dosing scenarios. Within comparative pharmacokinetics across species, these models are indispensable for translating preclinical findings into human dosing recommendations, ensuring that regimens are optimized not just for idealized conditions, but for the variable reality of clinical use [83] [88].
The common perception that QD dosing is superior due to better compliance is nuanced by pharmacometrics. While QD regimens often show a higher percentage of prescribed doses taken, the therapeutic impact of a missed dose is more severe than for a BID regimen. A single missed QD dose is pharmacokinetically equivalent to two to three sequentially missed BID doses. Research indicates the probability of such sequential BID omissions is about half that of missing a single QD dose, suggesting that under certain conditions, a BID regimen could better maintain drug concentrations within a therapeutic window [88] [89]. This highlights the critical need for drug-specific modeling to determine the optimal regimen, considering not just compliance rates but the full pharmacokinetic and pharmacodynamic profile [88].
Theoretical Foundation: PK/PD Modeling in Regimen Selection
Core Pharmacokinetic and Pharmacodynamic Concepts
PK/PD modeling integrates two fundamental components: Pharmacokinetics (PK), which describes what the body does to the drug (absorption, distribution, metabolism, excretion), and Pharmacodynamics (PD), which describes what the drug does to the body (the biochemical and physiological effects) [90]. These elements are integrated into a single model that predicts the time course of effect intensity in response to a drug regimen [91].
Key PK parameters critical for dosing regimen optimization include:
- Area Under the Curve (AUC): A measure of total drug exposure over time.
- Maximum Concentration (Cmax): The peak plasma concentration.
- Minimum Concentration (Cmin): The trough plasma concentration, critical for maintaining efficacy.
- Time to Cmax (Tmax): The time taken to reach peak concentration.
- Half-life (t½): The time required for the plasma concentration to reduce by half.
The therapeutic window—the range between the minimum effective concentration and the minimum toxic concentration—is the primary target for any dosing regimen. The goal of QD vs. BID optimization is to maintain plasma concentrations within this window throughout the dosing interval, minimizing fluctuations that could lead to sub-therapeutic effects or toxicity [83].
From Empirical to Mechanistic Modeling Approaches
PK/PD modeling has evolved from empirical approaches to more sophisticated mechanistic models.
- Empirical (Hill-Based) Models: These models, such as the sigmoidal Emax model, use mathematical functions to describe the relationship between drug concentration and effect. They are useful for summarizing data but offer limited insight into the underlying biological processes. They often assume rapid equilibrium between drug and target, which can be a limitation for drugs with slow binding kinetics [90].
- Mechanistic Models: These models explicitly incorporate the biology of the system, including the kinetics of drug-target interaction, target occupancy, and target turnover. They are particularly valuable for predicting the impact of binding kinetics on a drug's duration of action and for understanding complex scenarios like prodrug activation or multi-drug therapies [91] [90]. By integrating target vulnerability functions, these models can define the precise relationship between target occupancy and the resulting pharmacological effect, providing a deeper understanding of the drug's mechanism of action [90].
Methodology: A Framework for QD vs. BID Modeling
Experimental and Data Requirements
Robust PK/PD modeling requires high-quality, comprehensive data. The following table outlines the essential data inputs and their roles in the modeling process.
Table 1: Essential Data Inputs for QD/BID PK/PD Modeling
| Data Category | Specific Requirements | Purpose in Modeling |
|---|---|---|
| Preclinical PK Data | Plasma, blood, or tissue concentration-time data from one or more species [91]. | To characterize the fundamental ADME properties of the drug and establish interspecies scaling relationships. |
| In Vitro ADME Data | In vitro metabolism, permeability, and protein binding data for preclinical species and human [91]. | For In Vitro-In Vivo Extrapolation (IVIVE) to predict human PK parameters. |
| Drug Activity Data | In vitro potency (e.g., EC50) and in vivo efficacy data from animal models [91] [92]. | To establish the Pharmacodynamic (PD) relationship between concentration and effect. |
| Physicochemical Properties | Compound structure (SDF or SMILES file), lipophilicity, solubility [91]. | To inform distribution and absorption models, particularly in PBPK approaches. |
| Clinical Data (if available) | Phase I single ascending dose (SAD) and multiple ascending dose (MAD) PK data [83]. | To build and validate the core PK model for human dose and regimen prediction. |
PK Sampling Strategy
A well-designed PK sampling schedule is crucial for accurately capturing a drug's concentration-time profile. Regulatory agencies recommend collecting 12 to 18 samples per subject (including a pre-dose sample) across a dosing interval, continuing for at least three terminal elimination half-lives to fully characterize the absorption, distribution, and elimination phases [93]. For QD vs. BID comparisons, sampling must be intensive enough to capture the different fluctuation profiles, with particular attention to Cmax and Cmin values. In later-stage trials, sparse sampling strategies combined with population PK (popPK) modeling can be employed, especially in patient populations where extensive sampling is not feasible [93].
Model Development and Workflow
The process of developing and applying a PK model for dosing regimen optimization is iterative and collaborative. The following diagram illustrates the core workflow, from data integration to regimen selection.
Figure 1: PK Modeling Workflow for Dosing Regimen Optimization.
The process is an interactive one between the client and modeling experts, typically starting with an assessment of all available in vitro and in vivo data [91]. As shown in Figure 1, this data feeds into the development of a PK model, which is then linked to a PD model to understand the effect timeline. This integrated PK/PD model is used to simulate QD and BID dosing scenarios at steady-state. The outputs—including key parameters like AUC, Cmax, and Cmin—are analyzed to determine which regimen best maintains concentrations within the therapeutic window, factoring in real-world considerations like patient compliance [83] [88].
Case Study Analysis: QD vs. BID Decision in Practice
Scenario and Quantitative Outcomes
A real-world application from Premier Research demonstrates the power of this approach. The sponsor needed to select a dosing regimen for a Phase 2 study, debating between a BID and a more patient-friendly QD schedule. Using PK data from a Phase 1 single ascending dose (SAD) study, modelers simulated steady-state exposure for both regimens [83].
The results, summarized in the table below, provided a clear, quantitative comparison.
Table 2: Simulated Steady-State PK Parameters for QD vs. BID Dosing [83]
| PK Parameter | BID Regimen | QD Regimen | Clinical Interpretation |
|---|---|---|---|
| AUC (hr·ng/mL) | 1896 | 1893 | Equivalent total drug exposure. |
| Css,avg (ng/mL) | 79 | 78 | Equivalent average concentration. |
| Cmax at steady-state | Lower | ~2x higher (vs. BID) | Potential safety flag for drugs with a narrow therapeutic index. |
| Cmin at steady-state | Higher | Lower (greater drop) | Potential efficacy risk if trough falls below therapeutic level. |
Interpretation and Decision Drivers
The modeling revealed that while overall exposure (AUC) and average concentration were equivalent between the two regimens, the peak-to-trough fluctuation was significantly different [83]. The QD regimen produced a Cmax that was double that of the BID regimen. For a drug with a narrow therapeutic index, such a high peak could pose a safety concern (toxicity). Conversely, the lower Cmin with QD dosing could increase the risk of sub-therapeutic effects at the end of the dosing interval.
In this specific case, the higher Cmax was not deemed a safety concern based on the drug's profile. Therefore, the sponsor confidently proceeded with the QD regimen, prioritizing the demonstrated benefit of improved patient compliance without sacrificing efficacy [83]. This decision was made without the need for a costly and time-consuming preliminary multiple-dose trial, showcasing how modeling can de-risk and accelerate development.
Successful PK/PD modeling relies on a combination of specialized software, data, and expertise.
Table 3: Essential Resources for PK/PD Modeling and Dosing Optimization
| Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Modeling Software | NONMEM, Phoenix NLME, Monolix [94] | Industry-standard software for performing population PK/PD analysis using nonlinear mixed-effects modeling. |
| Simulation Platforms | Simcyp Simulator, GastroPlus, PK-Sim [95] | Advanced platforms that facilitate PBPK modeling, allowing for IVIVE and prediction of PK in virtual populations. |
| Bioanalytical Reagents | LC-MS/MS Assays, Validated Biomarker Kits [93] [92] | Critical for generating high-quality concentration and biomarker data from plasma, serum, or tissue samples. |
| Data Management | Electronic Data Capture (EDC) systems | Ensure accurate and reliable capture of dosing history and sample collection times, which is crucial for model integrity [93]. |
| Reference Compounds | Tool compounds with established PK/PD [92] | Used to validate and refine preclinical disease models before testing novel chemical entities. |
This case study underscores that the choice between QD and BID dosing is a complex trade-off that must be evaluated on a drug-by-drug basis. PK modeling and simulation provide an indispensable, quantitative framework for making this critical development decision. By simulating steady-state exposure, the model highlights key differences in Cmax and Cmin fluctuations that are not apparent from single-dose data alone [83]. Furthermore, integrating an understanding of real-world compliance patterns—where the impact of a single missed QD dose can be more detrimental than missing one BID dose—enables the selection of a regimen that is not only effective in a controlled trial but also robust in clinical practice [88] [89]. As a cornerstone of comparative pharmacokinetics, this model-informed approach de-risks drug development, optimizes resource allocation, and ultimately helps deliver safer and more effective dosing regimens to patients.
Handling Species-Specific Metabolism and Active Metabolite Formation
In drug development, accurately predicting how a drug will behave in humans based on animal studies is a fundamental challenge. Species-specific differences in metabolic pathways and the formation of active metabolites can significantly influence drug efficacy, toxicity, and dosing regimens. Understanding these differences is crucial for translational research, helping to optimize preclinical models and improve the safety profile of investigational drugs. This guide objectively compares metabolic handling across species, using trazodone and other case studies to illustrate key principles in comparative pharmacokinetics.
Quantitative Comparison of Species-Specific Metabolic Parameters
The metabolism of drugs varies significantly between species, impacting the interpretation of preclinical data. The tables below summarize key quantitative differences for specific drugs.
Table 1: Species-Specific Metabolic Parameters for Trazodone [96]
| Parameter | Human | Mouse | Rat |
|---|---|---|---|
| Primary Metabolizing Enzyme | CYP3A4 | CYP3A | CYP3A |
| Key Active Metabolite | mCPP | mCPP | mCPP |
| Formation of mCPP | CYP3A4-mediated | CYP3A-mediated | CYP3A-mediated |
| Other Contributing Enzymes | CYP2D6, CYP2C19, FMOs | Information not specified in source | Information not specified in source |
| Hepatic Intrinsic Clearance | Slowest | Faster than human | Faster than human |
Table 2: Species-Specific Metabolic Parameters for Vicagrel [97]
| Parameter | Human | Dog | Rat |
|---|---|---|---|
| Systemic Exposure to Active Metabolite (AM) | Information not specified in source | 635.1 μg⋅h/L | 99.0 μg⋅h/L |
| Systemic Exposure to Inactive Metabolite (CAM) | Information not specified in source | 2634 μg⋅h/L | 10119 μg⋅h/L |
| Intestinal Hydrolytic Clearance | Information not specified in source | 3.643 Lâ‹…hâ»Â¹â‹…kgâ»Â¹ | 53.28 Lâ‹…hâ»Â¹â‹…kgâ»Â¹ |
| Esterase Activity in Plasma | No carboxylesterases (CEs) | No carboxylesterases (CEs) | High, contains CEs |
| Esterase Activity in Intestine | CE2 predominantly expressed | Almost none | CE2 predominantly expressed |
Experimental Protocols for Metabolic Pathway Characterization
Hepatic Metabolic Stability Assessment
This protocol is used to determine the intrinsic clearance of a compound and identify metabolic differences across species [96].
- Test System Preparation: Obtain cryopreserved hepatocytes from human, mouse, and rat sources. Pool cells from multiple donors to account for population variability. The final concentration should be approximately 0.5 million cells/mL in William’s medium E supplemented with glutamine and HEPES.
- Compound Incubation: Prepare the test compound (e.g., trazodone hydrochloride) at a final concentration of 10 µM. Incubate the compound with the hepatocyte suspension in duplicate at 37°C for up to 180 minutes.
- Sample Collection and Termination: Collect samples at designated time points (e.g., 0, 5, 10, 15, 20, 30, 45, 60, 90, 120, 150, and 180 minutes). Terminate the reactions by adding acetonitrile at a 1:2 ratio to precipitate proteins.
- Analysis: Centrifuge the terminated samples and analyze the supernatants using Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS). Monitor the disappearance of the parent compound over time to calculate the first-order elimination constant (k) and subsequent intrinsic clearance.
Identification of Metabolizing Enzymes Using Recombinant Systems and Inhibitors
This methodology identifies the specific cytochrome P450 (CYP) isoforms responsible for a drug's metabolism [96].
- Recombinant Enzyme Assay: Incubate the drug with individual, expressed recombinant human CYP enzymes (e.g., CYP3A4, CYP2D6, CYP2C19).
- Chemical Inhibition Assay: Incubate the drug with human liver microsomes in the presence of selective chemical inhibitors for specific CYP isoforms (e.g., ketoconazole for CYP3A4).
- Metabolite Analysis: In both assays, use LC-MS/MS to quantify the formation of specific metabolites (e.g., mCPP from trazodone). Significantly higher metabolite formation in a specific recombinant CYP system, or significant inhibition of metabolite formation by a specific chemical inhibitor, identifies the primary enzyme responsible for that metabolic pathway.
In Vitro Investigation of Hydrolytic Metabolism
This protocol is critical for prodrugs or compounds susceptible to esterase-mediated hydrolysis, as demonstrated in vicagrel studies [97].
- Matrix Preparation: Prepare pooled plasma, intestinal microsomes, and hepatic microsomes from the species of interest (e.g., rat, dog, human).
- Hydrolysis Reaction: Incubate the test compound with the different matrices under physiological conditions (e.g., 37°C, appropriate pH buffer).
- Metabolite Quantification: At designated time points, terminate the reaction and use LC-MS/MS to measure the formation of hydrolysis metabolites (e.g., the inactive carboxylic acid metabolite). This allows for the calculation of hydrolytic clearance in each matrix and the comparison of esterase activity across species.
Metabolic Pathways and Experimental Workflows
The following diagrams illustrate the key metabolic pathways and standard experimental workflows used in this field.
Trazodone Metabolic Pathway
Cross-Species Metabolic Comparison Workflow
The Scientist's Toolkit: Key Research Reagents and Materials
Successful investigation of species-specific metabolism requires a suite of specialized reagents and systems. The following table details essential materials and their functions.
Table 3: Essential Research Reagents for Metabolic Studies
| Reagent / Material | Function & Application |
|---|---|
| Cryopreserved Hepatocytes | Primary cells used to assess hepatic metabolic stability and intrinsic clearance across different species (human, rat, mouse) [96]. |
| Liver and Intestinal Microsomes | Subcellular fractions containing drug-metabolizing enzymes; used for high-throughput screening of metabolic pathways and enzyme kinetics [97]. |
| Recombinant CYP Enzymes | Individually expressed human cytochrome P450 isoforms; used to identify the specific enzyme(s) responsible for metabolizing a drug [96]. |
| Selective Chemical Inhibitors | Compounds that inhibit specific CYP enzymes (e.g., ketoconazole for CYP3A4); used to confirm the role of an enzyme in a metabolic pathway [96]. |
| LC-MS/MS System | Analytical platform (e.g., Agilent HPLC coupled to Sciex mass spectrometer) for sensitive and specific quantification of drugs and their metabolites in complex biological matrices [96]. |
Validation Frameworks and Regulatory Considerations in Comparative PK
Incurred Sample Reanalysis (ISR) is a critical quality assessment tool in regulated bioanalysis, used to verify the reproducibility and reliability of bioanalytical methods applied to samples from dosed subjects [98]. Unlike validation exercises that use spiked quality control (QC) samples, ISR assesses a method's performance with incurred samples, which contain the parent drug, its metabolites, and other endogenous components that can more accurately represent study sample composition [99] [98]. This distinction is vital because QC samples may not fully mimic the behavior of analytes in incurred samples due to factors such as metabolite back-conversion, protein binding effects, and sample inhomogeneity [98].
The practice of ISR has evolved from a scientific recommendation to a regulatory requirement in both clinical and non-clinical studies [98] [100]. Its importance was solidified following discussions at AAPS/FDA workshops, which highlighted cases where analytical methods demonstrated significant variability when analyzing incurred samples despite successful validation with QC samples [98]. For researchers engaged in comparative pharmacokinetics across species, ISR provides assurance that bioanalytical data—which forms the basis for critical decisions in drug development—is reliable and reproducible across diverse biological matrices and species [101].
Regulatory Framework and Acceptance Criteria
Global regulatory authorities, including the FDA, European Medicines Agency (EMA), and Health Canada, have established specific guidelines for ISR implementation [98] [100]. These guidelines provide a framework for demonstrating assay reproducibility, which is particularly important for pivotal studies such as bioequivalence, pharmacokinetic, and toxicokinetic investigations [102] [98].
Table 1: ISR Requirements Across Regulatory Guidelines
| Regulatory Agency | ISR Requirement | Sample Selection | Acceptance Criteria |
|---|---|---|---|
| FDA | Required for pivotal PK/PD and human bioequivalence studies; at least once for each method and species during non-clinical safety studies [98] | Up to 10% of study samples, covering the entire PK profile including C~max~ and elimination phase [98] | ≥67% of results within 20% of original for small molecules; within 30% for large molecules [98] |
| EMA | Applied to pre-clinical toxicokinetic and clinical pharmacology studies [100] | Not specified in detail, but should represent the full concentration-range and time-points [100] | Consistent with FDA (≥67% within 20%/30%) [100] |
| Global Bioanalysis Consortium (GBC) | Recommended for critical studies including bioequivalence trials [102] | Samples should represent full concentration range, avoiding those near the limit of quantitation [102] | At least 66.7% of results must meet acceptance criteria [102] |
The acceptance criterion—requiring at least two-thirds (67%) of repeated results to be within 20% of the original value for small molecules and 30% for large molecules—represents a harmonized standard across major regulatory bodies [102] [98] [100]. This criterion applies to the percentage difference, calculated as: (Repeat - Original) × 100 / Mean [98].
ISR Experimental Protocol and Workflow
Implementing ISR requires a systematic approach that begins during method development and continues through study sample analysis. The following workflow outlines the key stages in executing a proper ISR assessment.
Diagram 1: ISR Implementation Workflow
Sample Selection Criteria
The selection of appropriate samples for ISR is crucial for obtaining meaningful results. Regulatory guidelines and best practices recommend [102] [98]:
- Selecting samples that represent the entire pharmacokinetic profile, including time points around C~max~ and during the elimination phase
- Choosing samples from individual subjects rather than pooled samples
- Ensuring coverage of the full concentration range, avoiding samples with concentrations near the lower limit of quantitation where variability is typically higher
- Including approximately 5-10% of total study samples, with regulatory guidelines often specifying 10% for studies with up to 1000 samples and 5% for larger studies [98] [103]
Analytical Execution
The reanalysis must be conducted using the original bioanalytical method without modification, including the same number of replicates and any applied dilution factors [98]. The analysis should be performed against freshly prepared calibrators to ensure independence from the original analysis [98]. Samples should be reanalyzed in a separate run on a different day to confirm the reproducibility of the method over time [98].
Essential Research Reagents and Materials
Successful ISR implementation requires specific laboratory materials and reagents that ensure the reliability and reproducibility of bioanalytical methods.
Table 2: Essential Research Reagent Solutions for ISR
| Reagent/Material | Function in ISR | Key Considerations |
|---|---|---|
| Blank Biological Matrix | Used for preparation of calibration standards and quality control samples [98] | Should be from the same species and tissue type as incurred samples; free of interfering substances [98] |
| Reference Standard (Analyte) | For preparing calibration curves and QC samples [98] | High purity with documented identity and stability; should match the drug substance in incurred samples [98] |
| Stable-Labeled Internal Standard | Used to correct for variability in sample preparation and analysis [98] | Ideally deuterated or otherwise isotopically labeled; should behave similarly to the analyte throughout the analytical process [98] |
| Sample Processing Reagents | For protein precipitation, extraction, or purification [99] | Optimization required during method validation; pH adjustment may be critical for metabolite stability [99] |
| Mobile Phase Components | For chromatographic separation in LC-MS/MS methods [98] | Buffer pH and composition must be controlled to ensure reproducibility between original and reanalysis [99] |
Case Studies in ISR Implementation
Troubleshooting ISR Failure: Capecitabine Metabolite Analysis
A compelling case study involves the analysis of capecitabine and its metabolite 5-fluorouracil (5-FU) [98]. Initially, ISR passed for the parent drug but failed for the metabolite, with highly variable 5-FU concentrations observed during reanalysis. Investigation revealed that the instability of intermediate metabolites (5'-DFCR and 5'-DFUR) in blood and plasma led to continued conversion to 5-FU after sample collection [98]. This case highlights how sample handling stability issues that may not be apparent during initial method validation can be uncovered through ISR.
Impact of Sample Processing Environment
Another case study identified an ISR failure related to a change in laboratory environment during the analysis of mesalamine [99]. The investigation traced the problem to variations in buffer pH during sample preparation, which significantly impacted analyte recovery and measurement reproducibility [99]. This example underscores the importance of controlling environmental factors and maintaining consistent sample processing conditions between original analysis and reanalysis.
Statistical Considerations and Sample Size
The appropriate number of samples for ISR has been the subject of ongoing scientific discussion. While current FDA and EMA guidelines recommend reanalyzing 7-10% of study samples, recent research suggests that a fixed number of samples (e.g., 30-50) might provide more consistent statistical power across studies of different sizes [103].
Statistical analysis using the hypergeometric distribution has demonstrated that fixed sample sizes (rather than percentages) may offer better discrimination between reproducible and non-reproducible methods, particularly for smaller studies [103]. This approach acknowledges that the probability of passing ISR depends not only on the method's true performance but also on the number of samples reanalyzed.
ISR in Comparative Pharmacokinetics Across Species
In comparative pharmacokinetics, where studies often span multiple species with different metabolic profiles and matrix compositions, ISR takes on additional importance [101]. Physiological differences between species can lead to variable matrix effects, differential metabolite profiles, and distinct protein binding characteristics that may affect analytical reproducibility [101].
The Global Bioanalysis Consortium emphasizes that ISR should be performed for each species during method validation, as matrix effects can be species-specific [102]. This is particularly critical for veterinary drugs, where international guidelines show some variation in bioequivalence requirements [101]. For researchers comparing pharmacokinetic profiles across species, successful ISR provides confidence that observed differences reflect true physiological variability rather than analytical artifacts.
Incurred Sample Reanalysis represents a critical component of bioanalytical method validation, providing essential verification of assay reproducibility under actual study conditions. By implementing rigorous ISR protocols following regulatory guidelines and best practices, researchers can ensure the reliability of pharmacokinetic data supporting drug development decisions. For comparative pharmacokinetic studies across species, where biological variability introduces additional complexity, ISR serves as a decisive tool for validating analytical methods and confirming the integrity of species-specific pharmacokinetic data.
Understanding the physiological differences between humans and canines is a critical component of comparative pharmacokinetics, with direct implications for human drug development and veterinary medicine. Pharmacokinetics (PK) describes how a drug is absorbed, distributed, metabolized, and excreted (ADME) by the body, and each of these processes can be significantly influenced by species-specific physiological factors [104] [25]. This knowledge is fundamental for translational research, particularly in areas like oncology and neurodegenerative diseases where dogs serve as valuable spontaneous models of human conditions [104] [105]. This guide provides a structured comparison of canine and human physiology affecting drug PK, supported by experimental data and methodologies.
Significant anatomical and physiological differences between dogs and humans lead to variations in how drugs behave in vivo. These differences must be understood to enable accurate extrapolation of drug behavior across species.
Table 1: Key Physiological and PK Parameters in Dogs and Humans
| Parameter | Canine | Human | Impact on Pharmacokinetics |
|---|---|---|---|
| Gastric pH (fasted) | ~2.0 [105] | ~1.5-2.0 [105] | Affects dissolution and stability of pH-sensitive drugs, influencing absorption. |
| Gastric Residence Time | Highly variable; shorter in fasted state [105] | Longer and more predictable [105] | Impacts the time available for a drug to dissolve and be absorbed in the stomach. |
| Intestinal pH (fasted) | Jejunum: ~7.3; Colon: ~7.0 [105] | Jejunum: ~6.5; Colon: ~7.5 [105] | Regional pH differences can alter the absorption profile of weakly acidic or basic drugs. |
| Bile Salt Composition | Different profile (e.g., higher deoxycholate) [105] | Distinct human-specific profile [105] | Influences the solubility of lipophilic drugs, thereby affecting absorption. |
| CYP Enzyme Abundance | Different isoform abundance and activity (e.g., CYP1A, CYP2B, CYP3A) [104] | Human-specific CYP profile (e.g., CYP3A4 dominant) [104] | A major source of interspecies variation in drug metabolism and clearance. |
| Primary Dosing Index | Body Weight [106] | Body Surface Area or Weight [107] | Impacts how doses are scaled from one species to another for efficacy and safety. |
The following diagram summarizes the major interspecies differences in the ADME pathway that are detailed in the subsequent sections.
Drug Absorption & Gastrointestinal Differences
Drug absorption is primarily determined by the gastrointestinal (GI) environment. Canine and human GI physiology differ in ways that directly impact the dissolution and absorption of orally administered drugs [105].
Key Experimental Findings:
- Gastric pH and Motility: Dogs have a less predictable fasted gastric pH and a different pattern of interdigestive myoelectric complexes (the "housekeeper" waves that clear the stomach) compared to humans. This leads to more variable and often shorter gastric residence times in fasted dogs [105].
- Intestinal Fluids: The composition of canine intestinal fluids, particularly bile salts, differs significantly from humans. Canine bile has a higher proportion of deoxycholate, which can affect the solubilization capacity for lipophilic drugs [105].
- Experimental Protocols: To study these differences, researchers use telemetric motility capsules (e.g., SmartPill) in both species to simultaneously measure pH, pressure, and temperature throughout the GI tract [105]. In vitro, simulated intestinal fluids tailored to canine (FaSSIF-canine) and human (FaSSIF-human) compositions are used in dissolution experiments to predict absorption differences [105].
Table 2: Experimental Models for Studying GI Absorption
| Experimental Model | Protocol Summary | Key Measured Endpoints |
|---|---|---|
| Telemetric Motility Capsule | Ingestion of a wireless capsule that transmits physiological data as it travels through the GI tract [105]. | Gastric emptying time, intestinal pH profiles, regional transit times, pressure patterns. |
| In Vitro Dissolution Testing | Drug dissolution in biorelevant media simulating fasted or fed state canine or human intestinal fluids [105]. | Dissolution rate and efficiency, supersaturation potential, precipitation behavior. |
| Heidelberg pH Capsule | Ingestion of a small capsule that radiotelemeters intragastric pH [105]. | Real-time fasted and fed state gastric pH. |
Drug Distribution & Plasma Binding
Once absorbed, a drug distributes throughout the body. The extent of distribution is influenced by factors such as plasma protein binding, tissue composition, and blood flow, which can vary between species.
Key Experimental Findings:
- Protein Binding: Species differences in the concentration and binding affinity of plasma proteins like albumin and α1-acid glycoprotein can lead to differences in the free (active) fraction of a drug [25].
- Tissue Access: Physiological barriers like the blood-brain barrier express drug transporters (e.g., P-glycoprotein) whose activity and abundance may differ, altering drug distribution to sensitive tissues [108].
Drug Metabolism & Enzyme Activity
Metabolism is a primary source of interspecies variation in PK. The cytochrome P450 (CYP) enzyme superfamily, in particular, shows significant differences in isoform expression and activity between dogs and humans [104].
Key Experimental Findings:
- CYP Isoforms: Dogs express different major CYP isoforms compared to humans. For instance, the CYP3A subfamily, which metabolizes a vast array of human drugs, is not the dominant subfamily in canine liver, where CYP1A and CYP2B activities are more prominent [104] [109].
- Case Study - Naringin: Pharmacokinetic studies of the flavonoid naringin reveal stark metabolic differences. After administration, the metabolic pathways and the resulting metabolite profiles in rats, dogs, and humans were all different, highlighting the complexity of interspecies extrapolation [109].
The following diagram illustrates the workflow for characterizing interspecies drug metabolism, a critical step in PK studies.
Drug Excretion & Renal Clearance
Renal excretion is a key route of elimination for many drugs and their metabolites. The glomerular filtration rate (GFR) and the activity of renal transporters are primary determinants of renal clearance.
Key Experimental Findings:
- Creatinine Clearance: In humans, carboplatin dosing is carefully adjusted based on estimated GFR (using creatinine clearance) to minimize toxicity [107]. A recent study in dogs established that plasma creatinine concentration is also a significant covariate for carboplatin clearance, suggesting similar personalized dosing could be beneficial in veterinary medicine [107].
- Case Study - Carboplatin: A population PK study in client-owned dogs receiving carboplatin (300 mg/m²) found that both plasma creatinine concentration and neutering status were significant covariates for the drug's clearance. This model successfully predicted the drug's exposure (AUC), which correlated with the degree of thrombocytopenia, a key toxicity [107].
Table 3: Population PK Study of Carboplatin in Dogs [107]
| Study Element | Description |
|---|---|
| Objective | To characterize carboplatin PK in client-owned dogs and identify covariates for dose individualization. |
| Population | 16 client-owned dogs with various neoplasms. |
| Dosing | 300 mg/m² via slow (20-min) intravenous infusion. |
| Sampling Design | Sparse sampling (3-4 plasma samples per dog) using a windows design. |
| Bioanalysis | Free carboplatin measured in plasma ultrafiltrate using HPLC-MS/MS. |
| Modeling Software | Non-linear mixed-effect modelling with Monolix. |
| Key Covariates | Plasma creatinine concentration (inverse relationship with clearance) and sterilization status. |
| Application | Model-predicted AUC was a better predictor of thrombocyte reduction than BSA-based dosing. |
The Scientist's Toolkit: Key Research Reagents & Materials
The following tools and reagents are essential for conducting comparative pharmacokinetic studies.
Table 4: Essential Reagents and Materials for Comparative PK Studies
| Research Tool / Reagent | Function in PK Research |
|---|---|
| LC-MS/MS Systems | High-sensitivity quantification of drugs and their metabolites in complex biological matrices like plasma, urine, and tissues [107]. |
| Simulated Intestinal Fluids | Biorelevant media (e.g., FaSSIF, FeSSIF) used for in vitro dissolution testing to predict in vivo absorption in different species [105]. |
| Liver Microsomes | Subcellular fractions containing metabolic enzymes (CYPs, UGTs) used for in vitro incubation studies to identify metabolic pathways and interspecies differences [109]. |
| Telemetric Motility Capsules | Ingestible devices that measure pH, pressure, and temperature in vivo to characterize GI conditions in conscious animals and humans [105]. |
| Population PK Software | Software platforms (e.g., Monolix, NONMEM) for analyzing sparse data from heterogeneous populations to identify sources of PK variability [106] [107]. |
| Validated Bioanalytical Assays | Methods rigorously tested for specificity, accuracy, and precision to ensure reliable concentration data for PK modeling [109] [107]. |
The physiological differences between canines and humans—from GI physiology and enzyme activity to renal function—profoundly impact drug pharmacokinetics. These differences are not merely academic; they have practical consequences for dose selection, predicting drug safety, and interpreting efficacy in both veterinary and human drug development. The case studies of enflicoxib, carboplatin, and naringin demonstrate that while empirical body surface area scaling is common, more mechanistic approaches like population PK modeling and physiologically based pharmacokinetic (PBPK) modeling provide a superior framework for rational interspecies extrapolation [106] [107] [108]. Acknowledging and systematically investigating these interspecies differences is therefore paramount for the success of translational research and the development of safe and effective therapeutics for all species.
Regulatory Guidelines for Cross-Species Extrapolation (FDA, EMA)
Cross-species extrapolation serves as a fundamental pillar in pharmaceutical development, enabling researchers to translate biological data from animal studies to human therapeutic applications. This practice is indispensable for predicting human pharmacokinetics (PK), pharmacodynamics (PD), and toxicological outcomes, thereby streamlining drug development and reducing reliance on extensive animal testing. The regulatory landscape governing these approaches is primarily shaped by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). While neither agency has published a standalone, comprehensive guideline exclusively titled "Cross-Species Extrapolation," their expectations and requirements are embedded within a complex framework of topic-specific guidance documents and reflection papers. Understanding this framework is critical for researchers and drug development professionals aiming to design robust, defensible, and successful regulatory submissions.
The regulatory philosophy of both agencies centers on the principle of "totality of evidence," where extrapolation is justified not by a single study but by the integration of data from analytical, non-clinical, and, where necessary, clinical studies. A key concept in this domain is the "taxonomic domain of applicability," which refers to the understanding of biological conservation (or lack thereof) in pathways across species. This determines when data from one species can be reliably extrapolated to another [110]. Furthermore, agencies recognize advanced methodologies like Physiologically Based Pharmacokinetic (PBPK) modeling and allometric scaling as vital tools for informing these extrapolations, especially when supported by mechanistic data [111] [112].
Comparative Analysis of FDA and EMA Regulatory Approaches
The FDA and EMA both utilize cross-species extrapolation to enhance the efficiency of drug development, though their operational frameworks exhibit notable differences in centralization, specific therapeutic areas, and publicly available detail.
Table 1: Comparison of FDA and EMA Regulatory Frameworks for Extrapolation
| Aspect | U.S. Food and Drug Administration (FDA) | European Medicines Agency (EMA) |
|---|---|---|
| Guidance Accessibility | A single, searchable database of all guidance documents, filterable by topic (e.g., "Drugs," "Pediatric Product Development") [113]. | Guidance is dispersed across various committee-specific documents and scientific guidelines. |
| Pediatric Extrapolation | Referenced within the broader search framework; ICH E11 and E11(R1) are foundational [113]. | Explicitly addressed in the ICH E11A guideline, which provides a framework for using extrapolation in paediatric drug development [114]. |
| Biosimilar Extrapolation | Approves biosimilars with extrapolated indications, relying on the totality of evidence and clinical pharmacology similarities [115]. | Possesses a more defined framework for biosimilar extrapolation, though differences from the FDA approach can pose hurdles for developers [115]. |
| Key Document Types | Guidance Documents (Draft & Final), which can be general or product-specific. | Guidelines, Reflection Papers, and Scientific Advice procedures. |
A prominent example of regulatory harmonization is the ICH E11A guideline on paediatric extrapolation. This guideline provides a structured, iterative framework for using existing knowledge to extrapolate efficacy and safety data from adults to paediatric populations, thereby reducing the number of clinical trials required in children. It emphasizes understanding the disease similarity and exposure-response relationships between populations [114]. For biosimilars, both agencies practice extrapolation of indications, whereby a biosimilar can be approved for all indications of the reference product without generating separate clinical trial data for each condition. This practice is predicated on demonstrating comprehensive analytical similarity and a thorough justification based on the totality of evidence [115].
Foundational Scientific Methodologies and Data Requirements
The regulatory acceptance of any cross-species extrapolation is contingent upon a robust scientific foundation. Key methodologies include allometric scaling, PBPK modeling, and the use of the Adverse Outcome Pathway (AOP) framework.
Allometric Scaling
Allometric scaling is a well-established technique for predicting pharmacokinetic parameters in humans from animal data based on body weight. A meta-analysis of 85 veterinary drugs found that 77% showed significant correlations between total systemic clearance (CL) and body weight, while 88% showed significant correlations for volume of distribution at steady state (Vss) [112]. The mean allometric exponent (b) was 0.87 for CL and 0.99 for Vss. This study also highlighted that volume of distribution can often be predicted reliably using data from just two species, whereas the prediction of clearance typically requires data from three or more species for reliability [116] [112]. The identification of outlier species is a critical step in this process to avoid inaccurate predictions.
Physiologically Based Pharmacokinetic (PBPK) Modeling
PBPK modeling represents a more mechanistic and knowledge-driven approach. It incorporates species-specific physiology, plasma protein binding, and enzyme/transport kinetics to simulate drug disposition. A systematic evaluation demonstrated that the accuracy of cross-species PBPK extrapolations is significantly enhanced by incorporating species-specific physiology, enzyme/transporter kinetics, and tissue-specific gene expression profiles [111]. This synergistic use of data allows for a more confident prediction of human pharmacokinetics, directly supporting first-in-human trial design.
Adverse Outcome Pathway (AOP) Framework
The AOP framework provides a structured model for organizing toxicological data from the molecular initiating event to an adverse outcome at the organism level. Its utility in cross-species extrapolation lies in its ability to define the taxonomic domain of applicability of a pathway. By understanding the conservation of key events in an AOP across species, data from one species can be used to predict outcomes in another, mutually informing both human and environmental safety assessments [117] [110].
Table 2: Key Methodologies for Cross-Species Extrapolation
| Methodology | Core Principle | Typical Application | Data Requirements |
|---|---|---|---|
| Allometric Scaling | Empirical scaling of PK parameters based on body weight. | First-in-human dose estimation; veterinary drug development. | PK data (CL, Vss) from at least 3 animal species for reliable clearance prediction [116] [112]. |
| PBPK Modeling | Mechanistic modeling based on species-specific physiology and biochemistry. | Detailed prediction of human PK; investigation of drug-drug interactions; IVIVE. | Organ weights, blood flows, tissue composition, expression & activity of enzymes/transporters [111]. |
| AOP Framework | Organizing knowledge on the sequence of events leading to toxicity. | Ecological risk assessment; prioritizing chemicals for testing; justifying read-across. | Evidence for the conservation of molecular initiating events and key events across species [117] [110]. |
Experimental Protocols and Workflows
In Vitro to In Vivo Extrapolation (IVIVE) for Drug-Induced Liver Injury (DILI)
Modern approaches to de-risking preclinical development include sophisticated in vitro models that enable direct cross-species comparison. A leading-edge protocol involves using Liver-on-a-chip (microphysiological system) models derived from human, rat, and dog hepatocytes.
Detailed Protocol:
- Model Preparation: Seed primary hepatocytes from human, rat, or dog sources into the Liver-on-a-chip devices. Maintain them under perfused 3D culture conditions to promote high-level liver-specific functionality and longevity.
- Dosing Regimen: Expose the models to the drug candidate(s) of interest. This can involve single- or repeat-dosing over an experimental window of up to 14 days to uncover latent toxicities.
- Endpoint Analysis: Perform longitudinal and terminal assays to quantify DILI-specific biomarkers. These typically include:
- Clinical Chemistry: ALT, AST, GLDH for cytotoxicity.
- Functional Assays: Albumin secretion, urea synthesis, ATP content.
- Histological Assessment: Staining for bile canalicular architecture (e.g., MRP2), fat accumulation, and cell death.
- Data Integration and IVIVE: Compare the sensitivity and response profiles (e.g., IC50 values for cytotoxicity) across the human, rat, and dog models. This direct comparison flags interspecies differences early and provides a more comprehensive overview of the underlying mechanisms of hepatotoxicity, thereby improving the prediction of human-relevant DILI risk [118].
The workflow below illustrates the logical process of using cross-species data for predicting human outcomes, integrating both experimental and computational approaches:
Bioinformatic Analysis for Taxonomic Domain of Applicability
Justifying the relevance of an animal model for a specific drug target requires an understanding of evolutionary conservation. Bioinformatic tools are critical for this assessment.
Detailed Protocol:
- Target Identification: Define the primary molecular target (e.g., receptor, enzyme) of the drug.
- Sequence Retrieval: Obtain the protein sequence of the target from a reference species (e.g., human) and potential test species (e.g., mouse, rat, dog, non-human primate).
- Conservation Analysis: Use bioinformatic tools to assess conservation.
- SeqAPASS (Sequence Alignment to Predict Across Species Susceptibility): This publicly available tool compares the primary sequence, functional domain, and 3D homology of a protein across species to predict its potential susceptibility to chemical interaction [110].
- ExpressAnalyst (EcoOmics Analyst): A cross-species platform for RNAseq annotation and visualization that can be used to compare expression profiles of targets and related pathways in species with or without reference genomes [110].
- Interpretation: A high degree of sequence and functional domain similarity increases confidence that a biological effect observed in the test species is relevant to humans. Conversely, significant differences may identify the species as an outlier and preclude its use for extrapolation [110].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successfully navigating cross-species extrapolation requires a suite of specialized tools and reagents. The following table details key solutions used in the field.
Table 3: Key Research Reagent Solutions for Cross-Species Extrapolation Studies
| Tool/Reagent | Function in Research | Application Example |
|---|---|---|
| PhysioMimix DILI Assay | An organ-on-a-chip system that supports long-term (14-day) culture of primary hepatocytes in a 3D, perfused microenvironment for predictive toxicology studies. | Comparative studies of hepatotoxicity using human, rat, and dog liver models to flag interspecies differences early in development [118]. |
| Primary Hepatocytes (Human, Rat, Dog) | The core cellular component for liver MPS models; used to generate species-specific metabolic and toxicological response data. | Sourcing from reputable providers is critical for ensuring high metabolic function in IVIVE studies [118]. |
| SeqAPASS Tool | A bioinformatic tool that predicts protein susceptibility and taxonomic applicability by comparing sequence and functional domain homology across species. | Determining the conservation of a drug target (e.g., a receptor) across test species to justify model selection for toxicology studies [110]. |
| PBPK Modeling Software | Computational platforms (e.g., GastroPlus, Simcyp, PK-Sim) that simulate ADME processes by incorporating physiological, genetic, and biochemical parameters. | Building a rat PBPK model for a drug and then extrapolating it to human by replacing species-specific system parameters [111]. |
| EcoToxChip | A toxicogenomics tool using a standardized panel of genes to assess molecular responses to chemical exposure, aiding in chemical prioritization. | Screening for potential ecological risks by evaluating pathway-level effects across different species [117]. |
The relationship between these tools and the scientific workflow is illustrated below, showing how they generate data that feeds into the overall extrapolation strategy:
The regulatory guidelines for cross-species extrapolation, as implemented by the FDA and EMA, are evolving towards a more mechanistic and evidence-based paradigm. The core principles emphasized by both agencies are the totality of evidence, a deep understanding of the biological conservation of drug targets and pathways, and the application of advanced quantitative methods like PBPK modeling and bioinformatics. For researchers, the path to successful regulatory acceptance lies in proactively integrating these elements into drug development programs. Leveraging modern tools such as MPS for in vitro to in vivo extrapolation and bioinformatic analysis for taxonomic applicability will be crucial for generating the robust, defensible data required to justify extrapolations, ultimately leading to safer, more efficient, and more successful drug development.
Biomarker Validation and Correlation Across Species
Biomarker validation and correlation across species represents a critical frontier in comparative pharmacokinetics and drug development. This process establishes measurable biological indicators that can reliably translate findings from preclinical models to human clinical applications. In the context of comparative pharmacokinetics—which studies how drugs are absorbed, distributed, metabolized, and excreted (ADME) across different organisms—validated cross-species biomarkers provide essential bridges for predicting therapeutic efficacy and safety in humans [119] [9]. The fundamental challenge lies in establishing biomarkers that remain functionally consistent across species despite evolutionary divergence in physiological systems.
The validation continuum extends from initial analytical verification to comprehensive biological and cross-species validation [120]. Cross-species validation specifically assesses whether a biomarker maintains consistent functional relationships with biological processes of interest across multiple species, leveraging the concept that phylogenetically conserved pathways are more likely to represent universal biological mechanisms [120]. This approach is particularly valuable when biomarkers lie within causal pathways rather than merely representing associative phenomena, strengthening their predictive power in translational research.
Biomarker Categories and Their Cross-Species Applications
Biomarkers serve distinct functions throughout the drug development pipeline, each with specific implications for cross-species correlation. Understanding these categories ensures appropriate selection and interpretation during translational research.
Table 1: Biomarker Categories and Cross-Species Considerations
| Biomarker Category | Primary Function | Cross-Species Validation Emphasis |
|---|---|---|
| Diagnostic | Identify presence or absence of disease | Pathophysiological conservation of disease mechanisms |
| Prognostic | Predict disease outcome or progression | Conservation of disease progression pathways |
| Predictive | Identify likelihood of response to treatment | Target conservation and drug mechanism alignment |
| Pharmacodynamic/Response | Show biological response to therapeutic intervention | Conservation of drug-target interactions and downstream effects |
| Safety | Identify drug-induced toxicity | Conservation of toxicological pathways and metabolic activation |
| Monitoring | Track disease status or treatment response | Conservation of physiological response indicators |
Diagnostic biomarkers, such as prostate-specific antigen (PSA) for prostate cancer, require validation that the measured entity reflects similar pathophysiological processes across species [121]. Predictive biomarkers, like HER2/neu status in breast cancer, depend on conservation of both the target and the mechanism of action of the therapeutic intervention [121]. This categorical framework guides researchers in selecting appropriate biomarker types for specific cross-species translation goals within comparative pharmacokinetics studies.
Current Approaches to Cross-Species Biomarker Validation
Analytical and Biological Validation Foundations
Before cross-species correlation can be established, biomarkers must undergo rigorous analytical validation. This process assesses the accuracy, precision, sensitivity, specificity, and reproducibility of the measurement technique itself, independent of its biological significance [120] [122]. For biomarker assays, establishing quantitative ranges presents unique challenges compared to traditional drug assays because researchers must characterize endogenous molecules in biological samples rather than working with spiked samples of known reference standards [122].
Biological validation evaluates the extent to which a biomarker reflects fundamental knowledge about the biology of aging or disease processes [120]. This validation type determines whether the biomarker lies within causal pathways or merely represents associative phenomena. The conservation of biological mechanisms across species becomes particularly important at this stage, as biomarkers rooted in evolutionarily preserved pathways typically demonstrate greater translational reliability [120].
Methodological Frameworks for Cross-Species Correlation
Multiple reaction monitoring (MRM) profiling has emerged as a powerful high-throughput screening approach for cross-species biomarker discovery and validation. This methodology enables simultaneous monitoring of hundreds to thousands of precursor-fragment ion pairs without requiring full structural elucidation, significantly accelerating biomarker identification across species [123]. In boar fertility studies, MRM profiling identified 20 candidate biomarkers with area under the curve (AUC) values ≥0.800 (P<0.05), including kynurenine (AUC=0.905) for predicting post-thaw motility loss and guanosine (AUC=0.850) for predicting conception rate [123].
Table 2: Experimental Approaches for Cross-Species Biomarker Validation
| Methodology | Key Features | Applications in Cross-Species Research |
|---|---|---|
| Multiple Reaction Monitoring (MRM) Profiling | High-throughput screening of lipid and metabolite features; reduced instrument time | Identified candidate biomarkers predictive of boar cryotolerance and conception rates [123] |
| Multi-Omics Integration | Combined genomics, proteomics, metabolomics, and transcriptomics | Comprehensive biomarker signatures reflecting disease complexity across species [124] |
| Population Pharmacokinetic (PPK) Modeling | Identifies factors influencing pharmacokinetic variability across populations | Quantitative design of clinical trials; optimization of dosage across species [59] |
| Artificial Intelligence/Machine Learning | Predictive modeling of complex biomarker patterns | Forecasting disease progression and treatment responses across species [125] [124] |
Multi-omics approaches represent another powerful framework for cross-species biomarker validation. By integrating data from genomics, proteomics, metabolomics, and transcriptomics, researchers achieve a holistic understanding of disease mechanisms that facilitates identification of robust cross-species biomarker signatures [124]. This systems biology approach acknowledges the complexity of biological systems and enhances the likelihood of identifying evolutionarily conserved biomarkers with strong translational potential.
Technical Workflows and Visualization
The experimental workflow for cross-species biomarker validation follows a structured pathway from study design through analytical and clinical validation, with specific considerations for cross-species correlation at each stage.
The experimental workflow emphasizes standardized protocols across species to minimize technical variability that could confound cross-species comparisons [121] [120]. Data standardization and harmonization are particularly crucial when integrating datasets from multiple species with different biological matrices and analytical platforms. The iterative refinement process allows for continuous improvement of biomarker panels based on validation outcomes in successive species.
Key Signaling Pathways in Cross-Species Biomarker Research
Several evolutionarily conserved signaling pathways frequently serve as foundations for cross-species biomarker development in pharmacokinetics and disease research.
The cytochrome P450 enzyme system represents a critically important pathway for cross-species biomarker development in pharmacokinetics [9]. These enzymes, particularly CYP3A4, CYP2D6, and CYP2C9, metabolize approximately 70-80% of all pharmaceutical drugs and demonstrate species-specific variations in expression and activity that must be accounted for during biomarker validation [9]. Nuclear receptors such as PXR (pregnane X receptor) and CAR (constitutive androstane receptor) regulate these metabolic enzymes and provide additional targets for biomarker development that can bridge species differences in drug metabolism [9].
Research Reagent Solutions for Cross-Species Biomarker Studies
Cross-species biomarker validation requires specialized reagents and platforms designed to address the challenges of working with multiple species and complex biological matrices.
Table 3: Essential Research Reagents for Cross-Species Biomarker Validation
| Reagent/Platform | Function | Cross-Species Application |
|---|---|---|
| MRM Profiling Kits | Targeted quantification of metabolite and lipid panels | High-throughput screening of conserved metabolic pathways across species [123] |
| Cross-Reactive Antibodies | Immunodetection of conserved epitopes | Western blot, ELISA, and immunohistochemistry across multiple species |
| Multi-Species Genomic Arrays | Simultaneous measurement of gene expression | Conservation analysis of transcriptional responses across species |
| Population PK Modeling Software | Quantification of interspecies variability in drug disposition | NONMEM, Monolix for covariate identification across species [59] |
| Liquid Chromatography-Mass Spectrometry | Sensitive detection and quantification of biomarkers | Analysis of drugs and metabolites in complex biological matrices across species [123] [9] |
| AI-Predictive Analytics Platforms | Pattern recognition in complex multi-species datasets | Forecasting disease progression and treatment responses across species [125] [124] |
The selection of appropriate research reagents must consider cross-reactivity and specificity for intended species. Antibodies validated for multiple species improve comparability, while mass spectrometry-based approaches often provide greater consistency across species by focusing on conserved molecular mass rather than species-specific epitopes [123]. Liquid biopsy technologies are increasingly valuable for cross-species biomarker work, enabling real-time monitoring of disease progression and treatment responses through non-invasive sampling [124].
Biomarker validation and correlation across species remains a complex but essential component of comparative pharmacokinetics and translational drug development. Success requires integrated approaches that combine multi-omics technologies, sophisticated computational modeling, and rigorous validation frameworks. The continuing evolution of AI and machine learning applications in biomarker research promises enhanced capabilities for identifying conserved biological patterns across species [125] [124]. Population pharmacokinetic modeling has emerged as a particularly powerful tool for quantifying and explaining variability in pharmacokinetic parameters across species and populations [59].
Future progress will depend on collaborative frameworks that facilitate data sharing and standardization across research institutions and pharmaceutical companies [126]. As these technologies and frameworks mature, cross-species biomarker validation will increasingly enable model-informed precision dosing, improve preclinical to clinical translation, and accelerate the development of safer, more effective therapeutics across diverse populations.
Assessing Predictive Performance of PK Models for Clinical Translation
The transition of a drug candidate from preclinical research to clinical application is a high-attrition process, underscoring the critical need for robust predictive performance assessment of pharmacokinetic (PK) models. Model-informed drug development (MIDD) leverages quantitative frameworks to predict a drug's behavior in humans, directly impacting dosing strategy, safety profiling, and trial success rates [127]. This guide objectively compares established and emerging methodologies for evaluating PK model performance, with a specific focus on their application in cross-species translation. We present comparative data, detailed experimental protocols, and essential toolkits to aid researchers in selecting and applying the most appropriate validation strategies for their development programs.
Comparative Frameworks for Predictive Performance Assessment
The predictive performance of a PK model is evaluated through a combination of diagnostic metrics and visual tools. These methods assess how well model predictions align with observed experimental data, a process crucial for ensuring model reliability before clinical translation.
Key Diagnostic Metrics and Visual Tools
Core statistical metrics form the foundation of quantitative model assessment. Bias (or accuracy) indicates whether a model systematically over- or under-predicts observations, while precision measures the random scatter around the true values [128]. These are commonly calculated using the percentage prediction error (PE%) and absolute percentage prediction error (APE%) [128].
A powerful yet simple graphical approach involves plotting the ratio of Predicted to Observed drug concentrations versus time or versus the observed concentration itself [129]. This method readily reveals time- or concentration-dependent inaccuracies in the model's performance. The predictive performance can be quantified by the fraction of these concentration ratios that fall within an arbitrarily specified range, such as 0.8–1.2 (or 80% to 120%) [129].
For population PK (PopPK) models, goodness-of-fit (GOF) plots and prediction-corrected visual predictive checks (pcVPCs) are standard diagnostic tools. GOF plots, which include observations versus population or individual predictions, help identify model misspecification, while pcVPCs evaluate a model's ability to simulate data that match the central tendency and variability of the original observations [130].
Table 1: Key Diagnostic Metrics for PK Model Evaluation
| Metric Name | Calculation | Interpretation | Optimal Value |
|---|---|---|---|
| Median Prediction Error (MDPE) | Median of (Predicted - Observed)/Observed * 100% | Measure of bias or accuracy; systemic over- or under-prediction. | Close to 0% |
| Median Absolute Prediction Error (MDAPE) | Median of | (Predicted - Observed)/Observed | * 100% | Measure of precision; random scatter of predictions. | As low as possible |
| Root Mean Square Error (RMSE%) | SQRT( Mean( [ (Predicted - Observed)/Observed ]² ) ) * 100% | Composite measure of accuracy and precision. | As low as possible |
| Fraction within 0.8-1.2 Ratio | Percentage of (Predicted/Observed) ratios falling between 0.8 and 1.2 [129] | Direct measure of predictive performance. | High percentage (e.g., >80%) |
Case Studies in Model Evaluation and Translation
Antibody-Drug Conjugates (ADCs): T-DM1 Translation
A PK/PD modeling and simulation strategy was successfully applied for the clinical translation of trastuzumab emtansine (T-DM1) [127]. The methodology involved:
- Preclinical Model Development: A preclinical tumor disposition model for T-DM1 was used to characterize its in vivo efficacy in animal models, and efficacy parameters were estimated [127].
- Human PK Prediction: Human PK parameters were predicted using allometric scaling of monkey PK data [127].
- Clinical Translation & Validation: The predicted human PK, preclinical efficacy parameters, and clinical breast cancer parameters were combined into a translated clinical PK-PD model. This model was then used to simulate progression-free survival (PFS) and objective response rates (ORR), with the results showing comparability to outcomes observed in three separate clinical trials, thereby validating the approach [127].
This case demonstrates how a QSP model integrating in vitro cellular disposition, PK, and tumor growth inhibition data can be calibrated in xenograft mice and then translated to humans to successfully predict clinical efficacy [131].
Polymyxin B in Critically Ill Patients
An external evaluation of seven published PopPK models for intravenous Polymyxin B in critically ill patients provides a robust example of model validation [128]. The study assessed predictive performance using prediction-based (PE%, APE%) and simulation-based (pcVPC) diagnostics.
Table 2: External Validation Performance of Polymyxin B PopPK Models [128]
| Model Characteristic | Accuracy (MDPE) | Precision (MDAPE) | Key Finding from Ratio Plot | Suitability for MIPD |
|---|---|---|---|---|
| One-Compartment Models | Variable, generally higher bias | Variable, generally lower precision | Poor prediction of trough concentrations | Low |
| Two-Compartment Models | Lower bias | Higher precision | More accurately described the external validation dataset | High |
| Overall Finding | All models visually and statistically under-predicted plasma concentrations. | Two-compartment structures were superior. |
The study concluded that model performance was significantly influenced by the sampling strategy used in the original study, highlighting that models derived from well-informed, adequately powered clinical studies with appropriate sampling are more reliable for model-informed precision dosing (MIPD) [128].
Impact of Dataset Size on PopPK Model Evaluation
A 2025 study directly addressed whether a small real-world dataset could be effectively used for the external evaluation of a PopPK model, compared to a large virtual dataset [130]. Researchers evaluated a piperacillin/tazobactam model using data from only 13 patients versus a virtual population of 1000 patients.
The results demonstrated that the small clinical dataset revealed similar model misspecification in both GOF plots and pcVPCs as the large simulated dataset. Furthermore, no significant difference was found in the distributions of prediction errors between the two approaches [130]. This evidence supports that even small, well-structured clinical datasets can be sufficient for the external evaluation of PopPK models, a valuable finding for research in specialized or hard-to-recruit populations.
Experimental Protocols for Performance Assessment
Protocol for External Model Validation
This protocol is adapted from the Polymyxin B model evaluation study [128].
Independent Validation Data Collection:
- Population: Recruit patients from the target population (e.g., critically ill) not involved in the model's original development.
- Dosing & Sampling: Administer the drug and collect plasma samples at predefined times. Record exact dosing and sampling times.
- Covariates: Record key patient characteristics (e.g., weight, renal function, disease scores) required for the model's covariate relationships.
Model Implementation:
- Reproduce the published PopPK model in suitable software (e.g., NONMEM).
- Input the exact model structure, parameter estimates, covariate relationships, inter-individual variability, and residual error model as reported.
Prediction-Based Diagnostic:
- Use the implemented model to generate population predictions for each observed concentration in the validation dataset.
- Calculate PE% and APE% for each data point.
- Compute summary statistics: MDPE (for bias) and MDAPE (for precision).
Simulation-Based Diagnostic:
- Perform Monte Carlo simulations using the model and the validation dataset's dosing/covariate information.
- Generate prediction-corrected visual predictive checks (pcVPCs) to compare the simulated distributions with the observed data.
Graphical Analysis:
- Create a Predicted vs. Observed concentration ratio plot against time or observed concentration [129].
- Calculate the fraction of data points within the 0.8-1.2 ratio to quantify performance.
Protocol for Assessing Predictive Performance in Preclinical-Clinical Translation
This protocol is based on the strategy used for T-DM1 [127] and ADC QSP models [131].
Preclinical Model Development:
- Data: Collect robust in vivo PK and efficacy (e.g., tumor growth inhibition) data from animal models.
- Model Fitting: Develop a PK/PD model that characterizes the relationship between drug exposure and the efficacy endpoint. Estimate all relevant system and drug-specific parameters.
Human PK Prediction:
- Use allometric scaling or a PBPK approach to predict human PK parameters based on preclinical (e.g., monkey) PK data [127].
Clinical Translation of the Model:
Clinical Trial Simulation:
- Use the translated model to run virtual clinical trials.
- Simulate clinically relevant endpoints, such as progression-free survival (PFS) or objective response rate (ORR), for different dosing regimens or patient populations [127].
Model Validation:
- Compare the model-simulated outcomes with the results from actual clinical trials.
- Assess whether the model accurately predicts the magnitude of clinical effect and, ideally, differential efficacy across patient subpopulations (e.g., based on target expression levels) [131].
Figure 1: Workflow for Preclinical-to-Clinical PK/PD Model Translation and Validation. This diagram outlines the iterative process of developing a model from preclinical data, translating it for human predictions, and validating it against clinical trial outcomes.
Table 3: Key Software and Analytical Tools for PK Model Evaluation
| Tool Name/Type | Specific Examples | Primary Function in PK Assessment | Application Context |
|---|---|---|---|
| PopPK/QSP Software | nlmixr2 [132], NONMEM [128], Monolix |
Nonlinear mixed-effects modeling; parameter estimation; model simulation. | Core engine for building and evaluating PopPK and QSP models. |
| Bioanalytical Instrument | UHPLC-MS/MS [133] | Quantification of drug and metabolite concentrations in biological samples (e.g., plasma). | Generating the critical observed concentration data for model fitting and validation. |
| Statistical & Scripting Language | R [128], Python | Data management, statistical analysis, custom diagnostic plotting, and post-processing of model outputs. | Essential for calculating metrics, creating GOF plots, pcVPCs, and ratio plots. |
| Model Diagnostic Packages | xpose.nlmixr2 [132], ggPMX [132] |
Automated generation of goodness-of-fit and other diagnostic plots. | Streamlines model evaluation within R workflows. |
| Converter Tools | babelmixr2 [132], nonmem2rx [132] |
Convert models between different software formats (e.g., nlmixr2 to NONMEM/Monolix and vice-versa). | Facilitates model sharing and cross-platform evaluation. |
The rigorous assessment of predictive performance is not a mere regulatory checkbox but a fundamental component of robust PK model building and successful clinical translation. As demonstrated by the case studies, methodologies like external validation with ratio plots and clinical trial simulation provide tangible evidence of a model's utility. The choice of assessment strategy—from simple graphical checks to complex virtual trial simulations—should be guided by the model's intended purpose. The emerging consensus, supported by evidence, is that models incorporating mechanistic detail (e.g., two-compartment over one-compartment, QSP over empirical) and validated using relevant external data, even from small studies, provide the most reliable foundation for informing critical decisions in drug development, ultimately de-risking the journey from bench to bedside.
Conclusion
Comparative pharmacokinetics provides an essential bridge between preclinical discovery and clinical application, yet interspecies differences remain numerous and often unpredictable. Successful translation requires integrating fundamental physiological knowledge with advanced modeling approaches like PBPK and population PK, which account for variability and improve dosing predictions. The future of the field lies in expanding physiological databases, refining multi-scale models, and strengthening the quantitative framework for extrapolation, particularly for special populations and complex drug interactions. As these methodologies evolve, they will increasingly enable model-informed drug development, precision dosing across patient subpopulations, and more efficient advancement of safe, effective therapies from animals to humans. Collaborative efforts between academia, industry, and regulators will be crucial to standardize approaches and maximize the predictive power of comparative pharmacokinetic science.
References
- 1. Global Trends in Pharmacokinetic Changes... | Research Square [https://www.researchsquare.com/article/rs-7965704/v1]
- 2. In Vitro and In Vivo Assessment of ADME and PK Properties During Lead Selection and Lead Optimization – Guidelines, Benchmarks and Rules of Thumb - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK326710/]
- 3. Absorption, Distribution, Metabolism, and Excretion of US Food and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11022858/]
- 4. ADME Database : Fujitsu Global [https://www.fujitsu.com/global/solutions/business-technology/tc/sol/admedatabase/]
- 5. of the gastrointestinal Comparison , physiology, and... anatomy [https://pubmed.ncbi.nlm.nih.gov/8527686/]
- 6. tract ( Digestive ) | EBSCO Research comparative anatomy [https://www.ebsco.com/research-starters/anatomy-and-physiology/digestive-tract-comparative-anatomy]
- 7. Pharmacokinetics - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK557744/]
- 8. Drug Metabolism - Clinical Pharmacology - Merck Manual Professional Edition [https://www.merckmanuals.com/professional/clinical-pharmacology/pharmacokinetics/drug-metabolism]
- 9. Current trends in drug metabolism and pharmacokinetics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6900561/]
- 10. Model Accurately Predicts Dose Implications... | PNNL Pharmacokinetic [https://www.pnnl.gov/publications/pharmacokinetic-model-accurately-predicts-dose-implications-chemical-carcinogen]
- 11. - Across Meta-Analysis of Betamethasone Species ... Pharmacokinetics [https://pubmed.ncbi.nlm.nih.gov/41250930/]
- 12. Identification of Intestinal Loss of a Drug through Physiologically Based Pharmacokinetic Simulation of Plasma Concentration-Time Profiles | Clinical Pharmacokinetics [https://link.springer.com/article/10.2165/00003088-200847040-00003]
- 13. Pharmacokinetics and pharmacokinetic-pharmacodynamic correlations of therapeutic peptides - PubMed [https://pubmed.ncbi.nlm.nih.gov/23719681/]
- 14. Advance in peptide-based drug development: delivery platforms, therapeutics and vaccines | Signal Transduction and Targeted Therapy [https://www.nature.com/articles/s41392-024-02107-5]
- 15. and Molecular Modeling Indicate nAChRα4-Derived... Pharmacokinetics [https://pubmed.ncbi.nlm.nih.gov/34207317/]
- 16. Comparative Analysis of Experimental Pharmacokinetics of New Neurotropic Peptides | Biomedical Chemistry: Research and Methods [http://www.bmc-rm.org/index.php/bmcrm/article/view/92]
- 17. Pharmacokinetics, biodistribution and toxicology of novel cell-penetrating peptides | Scientific Reports [https://www.nature.com/articles/s41598-023-37280-0]
- 18. The influence of genetic in polymorphisms ... drug metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC7193447/]
- 19. Factors in Genetic | AAFP Drug Metabolism [https://www.aafp.org/pubs/afp/issues/2008/0601/p1553.html]
- 20. Clinical Pharmacogenetic Testing and Application: 2024 Updated Guidelines by the Korean Society for Laboratory Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788703/]
- 21. (PDF) Comparison of model-based tests and selection strategies to... [https://www.academia.edu/74356595/Comparison_of_model_based_tests_and_selection_strategies_to_detect_genetic_polymorphisms_influencing_pharmacokinetic_parameters]
- 22. Guidelines – CPIC [https://cpicpgx.org/guidelines/]
- 23. CPIC [https://cpicpgx.org/]
- 24. Species similarities and differences in pharmacokinetics - PubMed [https://pubmed.ncbi.nlm.nih.gov/8654187/]
- 25. Species differences in pharmacokinetics and pharmacodynamics - PubMed [https://pubmed.ncbi.nlm.nih.gov/20204582/]
- 26. Species differences in pharmacokinetics | Veterinary Research Communications [https://link.springer.com/article/10.1007/BF02228636]
- 27. , Pharmacodynamics, and... | Altasciences Pharmacokinetics [https://www.altasciences.com/resource-center/blog/pharmacokinetics-pharmacodynamics-and-toxicokinetics-demystified]
- 28. A Review on New Frontiers in Drug-Drug Interaction Predictions and Safety Evaluations with In Vitro Cellular Models [https://www.mdpi.com/1999-4923/17/6/747]
- 29. Exploring the Role of a Healthful Body in... - CVRTI Composition [https://cvrti.utah.edu/exploring-the-role-of-body-composition-in-cardiovascular-wellness/]
- 30. Gender Differences and Cardiovascular Drugs | Ten Points to... [https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2015/05/15/13/28/gender-differences-in-the-effect-of-cardiovascular-drugs]
- 31. AI-Derived Body Measurements Predict Cardiometabolic... Composition [https://www.acc.org/latest-in-cardiology/journal-scans/2025/10/08/13/30/ai-derived-body-composition]
- 32. The Impact of Body Composition on Cardiorespiratory Fitness in Adult Females - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10985563/]
- 33. Gender Differences in Hemodynamic Regulation and Cardiovascular Adaptations to Dynamic Exercise - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7393595/]
- 34. Cardiovascular and cardiorespiratory effects of high-intensity interval training in body fat responders and non-responders | Scientific Reports [https://www.nature.com/articles/s41598-024-65444-z]
- 35. between Difference & Population PBPK Modeling | Allucent PK [https://www.allucent.com/resources/blog/what-difference-between-pbpk-and-poppk-modeling]
- 36. Interacting Models, Real Drugs: Comparison of ML, PBPK , and... [https://pharmafeatures.com/interacting-models-real-drugs-comparison-of-ml-pbpk-and-pop-pk-for-pharmacokinetic-ddi-prediction/]
- 37. Physiologically based pharmacokinetic modelling - Wikipedia [https://en.wikipedia.org/wiki/Physiologically_based_pharmacokinetic_modelling]
- 38. PBPK modeling and simulation in drug research and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5125732/]
- 39. Recent Advances in Development and Application of Physiologically-Based Pharmacokinetic (PBPK) Models: a Transition from Academic Curiosity to Regulatory Acceptance | Current Pharmacology Reports [https://link.springer.com/article/10.1007/s40495-016-0059-9]
- 40. Premier Research | Choosing the Right PK Approach... Modeling [https://premier-research.com/perspectives/choosing-the-right-pk-modeling-approach-utilizing-nca-poppk-pd-and-pbpk-tools-for-midd-success/]
- 41. PBPK Modeling & Simulation in Drug Development [https://www.allucent.com/resources/blog/pbpk-modeling-and-simulation-drug-development]
- 42. the applications of machine learning, Comparing , and... PBPK [https://pmc.ncbi.nlm.nih.gov/articles/PMC9755922/]
- 43. Application of Physiologicallyâ€Based and Population Pharmacokinetic Modeling for Dose Finding and Confirmation During the Pediatric Development of Moxifloxacin - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6765696/]
- 44. Pediatric Pharmacokinetics and Dose Predictions: A Report of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7877839/]
- 45. The application of allometric principles to predict... scaling [https://pubmed.ncbi.nlm.nih.gov/24984569/]
- 46. What is Allometric & Its Role in Drug Development? Scaling [https://www.allucent.com/resources/blog/what-allometric-scaling-and-how-does-it-support-drug-development]
- 47. | PPTX Allometric scaling [https://www.slideshare.net/slideshow/allometric-scaling/62600878]
- 48. 异速生长 - 维基百科,自由的百科全书 [https://zh.wikipedia.org/zh-cn/%E5%BC%82%E9%80%9F%E7%94%9F%E9%95%BF]
- 49. All You Need to Know About Allometric : An Integrative... Scaling [https://link.springer.com/article/10.1007/s40262-024-01444-6]
- 50. (PDF) Allometric of scaling parameters in drug... pharmacokinetic [https://www.academia.edu/29213447/Allometric_scaling_of_pharmacokinetic_parameters_in_drug_discovery_Can_human_CL_Vss_and_t1_2_be_predicted_fromin_vivo_rat_data]
- 51. Allometric relationships between the pharmacokinetics of propofol in rats, children and adults - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1884857/]
- 52. 动物和人之间的剂é‡ä¸´åºŠå‰å’Œä¸´åºŠé˜¶æ®µå¦‚何转æ¢_检测资讯_嘉峪检测网 [http://m.anytesting.com/news/1935584.html]
- 53. An Update on the Use of Allometric and Other Scaling Methods to... [https://pubmed.ncbi.nlm.nih.gov/35018879/]
- 54. Application of Allometric Scaling to Nanochelator Pharmacokinetics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10399172/]
- 55. - Model ( Informed ) - PMC Precision Dosing MIPD [https://pmc.ncbi.nlm.nih.gov/articles/PMC9780803/]
- 56. Understanding Model-Informed Precision Dosing ( MIPD ) and Bayesian... [https://blog.insight-rx.com/resources/introduction-mipd-bayesian-pharmacy]
- 57. Frontiers | Software Tools for Model-Informed Precision Dosing: ... [https://www.frontiersin.org/articles/10.3389/fphar.2020.00620/full]
- 58. From Prospective Evaluation to Practice: Model - Informed ... Dose [https://link.springer.com/article/10.1007/s40265-025-02152-6]
- 59. Frontiers | Global research on the utilization of population... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1548023/full]
- 60. Predicting modelâ€informed precision dosing: A testâ€case in tacrolimus... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8923732/]
- 61. A continued learning approach for model - informed ... precision dosing [https://refubium.fu-berlin.de/handle/fub188/33850]
- 62. EDETEK Inc. | Edetek’s CONFORM Platform: Streamlining Clinical Data Management in Oncology Trials - EDETEK Inc. [https://edetek.com/edeteks-conform-platform-streamlining-clinical-data-management-in-oncology-trials/]
- 63. Edetek's CONFORM Platform: Streamlining Clinical Data Management in Oncology Trials - OncologyTube [https://oncologytube.com/edeteks-conform-platform-streamlining-clinical-data-management-in-oncology-trials/]
- 64. NIH Alzheimer’s Disease and Related Dementias 2025 ... Research [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 65. Analysis of Comparative Pharmacokinetics across Different... Posiphen [https://www.mdpi.com/2218-273X/14/5/582]
- 66. Comparative Analysis of Posiphen Pharmacokinetics across Different Species—Similar Absorption and Metabolism in Mouse, Rat, Dog and Human - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11117716/]
- 67. Comparative Analysis of Posiphen Pharmacokinetics across Different Species-Similar Absorption and Metabolism in Mouse, Rat, Dog and Human - PubMed [https://pubmed.ncbi.nlm.nih.gov/38785991/]
- 68. A multicenter, randomized, double-blind, placebo-controlled ascending... [https://alzres.biomedcentral.com/articles/10.1186/s13195-024-01490-z]
- 69. Buntanetap | ALZFORUM [https://www.alzforum.org/therapeutics/buntanetap]
- 70. Pharmacokinetics and Pharmacodynamics ( PK / PD ) Profile Analysis [https://umbrex.com/resources/industry-analyses/how-to-analyze-a-pharmaceutical-company/pharmacokinetics-and-pharmacodynamics-pk-pd-profile-analysis/]
- 71. Pharmacokinetics and Pharmacodynamics of Systemic Corticosteroids... [https://link.springer.com/article/10.1007/s40262-024-01419-7]
- 72. A systematic evaluation of the use of physiologically based... [https://pubmed.ncbi.nlm.nih.gov/25393841/]
- 73. - Cross of drug handling : Get Quote, RFQ, Price... species comparison [https://www.news-medical.net/Cross-species-comparison-of-drug-handling-with-near-physiological-kidney-transporter-model]
- 74. Use of normalized prediction distribution errors for assessing population physiologically-based pharmacokinetic model adequacy - PubMed [https://pubmed.ncbi.nlm.nih.gov/32323049/]
- 75. AI-Powered Prediction of Nanoparticle Pharmacokinetics ... [https://arxiv.org/html/2503.13798v1]
- 76. - Cross in nonclinical pharmacokinetics of... species comparison [https://www.nature.com/articles/s41598-023-35297-z?error=cookies_not_supported&code=76c985be-e896-4abc-bb37-305140dd78d3]
- 77. Narrow Therapeutic Index Drugs: FDA Experience, Views, and Operations - PubMed [https://pubmed.ncbi.nlm.nih.gov/39529254/]
- 78. 视频: 治 疗 指 数 [https://www.jove.com/cn/science-education/v/14431/therapeutic-index]
- 79. FY2015 Regulatory Science Research Report: Narrow Therapeutic Index Drugs | FDA [https://www.fda.gov/industry/generic-drug-user-fee-amendments/fy2015-regulatory-science-research-report-narrow-therapeutic-index-drugs]
- 80. Narrow Therapeutic Index Drug Pathways - BioPharma Services [https://www.biopharmaservices.com/blog/bioequivalence-drug-development-pathway-for-new-generic-narrow-therapeutic-index-drugs/]
- 81. Steady State Concentration - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK553132/]
- 82. Understanding Steady State Pharmacokinetics [https://www.certara.com/knowledge-base/understanding-steady-state-pharmacokinetics/]
- 83. Pharmacokinetic Modeling & Simulation to Optimize ... [https://premier-research.com/perspectives/increasing-clinical-trial-success-pharmacokinetic-modeling-simulation-to-optimize-dosing-regimens/]
- 84. Understanding PK Considerations for Repeat Dosing [https://www.allucent.com/resources/blog/pharmacokinetic-considerations-repeat-dosing]
- 85. Cross-species comparison in nonclinical pharmacokinetics ... [https://www.nature.com/articles/s41598-023-35297-z]
- 86. Two Innovative Approaches to Optimize Vancomycin Dosing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9147553/]
- 87. Meropenem dosing optimization on day 1 and steady state ... [https://www.nature.com/articles/s41598-025-20630-5]
- 88. Estimation of the comparative therapeutic superiority of QD and BID ... [https://link.springer.com/article/10.1007/s10928-007-9058-0]
- 89. Estimation of the comparative therapeutic superiority of QD and BID dosing regimens, based on integrated analysis of dosing history data and pharmacokinetics - PubMed [https://pubmed.ncbi.nlm.nih.gov/17497202/]
- 90. -Pharmacodynamic Pharmacokinetic that Incorporate... Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC7050630/]
- 91. PK/PD Modeling | Cyprotex ADME-Tox Solutions - Evotec [https://www.evotec.com/solutions/drug-discovery-preclinical-development/cyprotex-adme-tox-solutions/modeling-and-simulation/pk-pd-modeling]
- 92. Implementation of pharmacokinetic and pharmacodynamic strategies in early research phases of drug discovery and development at Novartis Institute of Biomedical Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4112793/]
- 93. Sampling PK : Importance, Schedule & Guidelines Optimization [https://www.allucent.com/resources/blog/why-pk-sampling-optimization-matters]
- 94. Basic Concepts in Population Modeling, Simulation, and Model-Based Drug Development—Part 2: Introduction to Pharmacokinetic Modeling Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636497/]
- 95. Basic Concepts in Physiologically Based Pharmacokinetic Modeling in Drug Discovery and Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3828005/]
- 96. Frontiers | Characterization of trazodone metabolic pathways and... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1636919/full]
- 97. of Pre-systemic Bioactivation of Vicagrel, a New... Species Comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC5054534/]
- 98. Incurred Sample Reanalysis, ISR Test | NorthEast BioLab [https://www.nebiolab.com/what-is-incurred-sample-reanalysis-isr/]
- 99. Incurred sample reanalysis ( ISR ): a decisive tool in bioanalytical research [https://pubmed.ncbi.nlm.nih.gov/21545349/]
- 100. Clinical pharmacology and pharmacokinetics : questions and answers [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/clinical-pharmacology-pharmacokinetics-questions-answers]
- 101. International Veterinary Bioequivalence Guideline Similarities and Differences Between Australia, Canada, Europe, Japan, New Zealand and the United States - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3475842/]
- 102. (PDF) Repeat Analysis and Incurred ... Sample Reanalysis [https://www.academia.edu/82862642/Repeat_Analysis_and_Incurred_Sample_Reanalysis_Recommendation_for_Best_Practices_and_Harmonization_from_the_Global_Bioanalysis_Consortium_Harmonization_Team]
- 103. : Time to Change the Incurred Size... Sample Reanalysis Sample [https://link.springer.com/article/10.1208/s12248-019-0293-2]
- 104. of Comparison and Canine Physiological Factors... Human [https://pubmed.ncbi.nlm.nih.gov/33907906/]
- 105. Comparison of Canine and Human Physiological Factors... [https://link.springer.com/article/10.1208/s12248-021-00590-0]
- 106. Frontiers | Enflicoxib for the long-term management of canine ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1645857/full]
- 107. Population pharmacokinetics modelling for clinical dose adjustment of... [https://bmcvetres.biomedcentral.com/articles/10.1186/s12917-024-04404-1]
- 108. Vinblastine pharmacokinetics in mouse, dog , and human in the... [https://scispace.com/papers/vinblastine-pharmacokinetics-in-mouse-dog-and-human-in-the-1b0xcxko]
- 109. Frontiers | Pharmacokinetics and Metabolism of Naringin and Active... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00364/full]
- 110. Cross Species Extrapolation [https://www.setac.org/explore-science/methods-and-approaches/cross-species-extrapolation.html]
- 111. A systematic evaluation of the use of physiologically based pharmacokinetic modeling for cross-species extrapolation - PubMed [https://pubmed.ncbi.nlm.nih.gov/25393841/?dopt=Abstract]
- 112. Interspecies allometric meta-analysis of the comparative pharmacokinetics of 85 drugs across veterinary and laboratory animal species - PubMed [https://pubmed.ncbi.nlm.nih.gov/25333341/]
- 113. Search for FDA Guidance Documents | FDA [https://www.fda.gov/regulatory-information/search-fda-guidance-documents]
- 114. ICH guideline E11A on pediatric extrapolation - Scientific guideline [https://www.ema.europa.eu/en/ich-guideline-e11a-pediatric-extrapolation-scientific-guideline]
- 115. Biosimilar Regulation: FDA and EMA Navigate Extrapolation of Indications as More Biosimilars Enter Market - GeneOnline News [https://www.geneonline.com/biosimilar-regulation-fda-and-ema-navigate-extrapolation-of-indications-as-more-biosimilars-enter-market/]
- 116. Interspecies scaling: a comparative study for the prediction of clearance and volume using two or more than two species - PubMed [https://pubmed.ncbi.nlm.nih.gov/8761347/]
- 117. Cross-Species Extrapolation of Biological Data to Guide the Environmental Safety Assessment of Pharmaceuticals-The State of the Art and Future Priorities - PubMed [https://pubmed.ncbi.nlm.nih.gov/37067359/]
- 118. CN Bio introduces cross - species DILI services to enhance in vitro to in... [https://www.news-medical.net/news/20250610/CN-Bio-introduces-cross-species-DILI-services-to-enhance-in-vitro-to-in-vivo-extrapolation-during-preclinical-drug-development.aspx]
- 119. Handbook of Comparative Pharmacokinetics and Residues of Veterinary Th [https://www.taylorfrancis.com/books/mono/10.1201/9781351072472/handbook-comparative-pharmacokinetics-residues-veterinary-therapeutic-drugs-arthur-craigmill]
- 120. of Validation of aging - PMC biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC11090477/]
- 121. Knowledge Graphs in Biomarker Discovery & Validation – Wisecube... [https://www.wisecube.ai/blog/knowledge-graphs-in-biomarker-discovery-validation/]
- 122. Understanding Biomarker Method Validation : Establishing... [https://www.linkedin.com/pulse/understanding-biomarker-method-validation-1ym5e]
- 123. Frontiers | A multi-omics approach identifies candidate biomarkers ... [https://www.frontiersin.org/journals/animal-science/articles/10.3389/fanim.2025.1665783/full]
- 124. Challenges and Future Trends in Biomarker Analysis for Clinical... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 125. Enhancing drug discovery with AI: Predictive modeling of pharmacokinetics using Graph Neural Networks and ensemble learning [https://journal.hep.com.cn/ip/EN/10.1016/j.ipha.2024.11.002]
- 126. Slow Aging, Extend Healthy Life | Federation of American Scientists [https://fas.org/publication/validation-biomarkers-endpoints/]
- 127. Application of a PK -PD Modeling and Simulation-Based Strategy for... [https://pubmed.ncbi.nlm.nih.gov/28374319/]
- 128. Assessing the predictive performance of population pharmacokinetic models for intravenous polymyxin B in critically ill patients - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8674003/]
- 129. Individual and population pharmacokinetic compartment analysis: a graphic procedure for quantification of predictive performance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4937653/]
- 130. Population Pharmacokinetic Model Evaluation with a Small Real-World... [https://pubmed.ncbi.nlm.nih.gov/40730936/]
- 131. Towards a platform quantitative systems pharmacology (QSP) model ... [https://link.springer.com/article/10.1007/s10928-023-09884-6]
- 132. Nonlinear Mixed Effects Models in Population PK/PD • nlmixr2 [https://nlmixr2.org/]
- 133. Frontiers | Comparison of the pharmacokinetic profiles of three... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1647015/full]