Bioavailability in Toxicity Testing: Bridging Exposure and Biological Effect for Accurate Risk Assessment
This article provides a comprehensive overview of the critical role bioavailability plays in modern toxicity testing.
Bioavailability in Toxicity Testing: Bridging Exposure and Biological Effect for Accurate Risk Assessment
Abstract
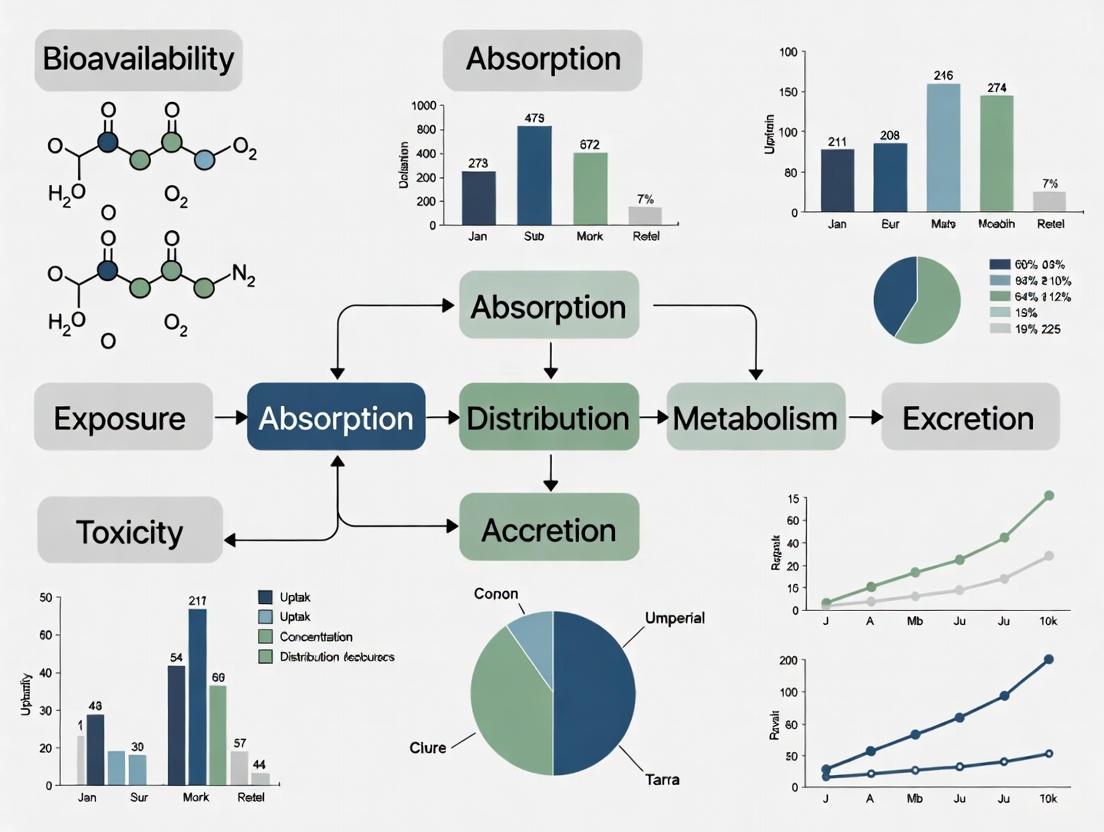
This article provides a comprehensive overview of the critical role bioavailability plays in modern toxicity testing. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles defining bioavailability and its necessity for accurate hazard identification. The scope covers established and emerging methodologies for assessing bioavailability across chemical and nanoparticle exposures, strategies for troubleshooting common limitations, and the application of bioavailability data in regulatory bioequivalence and comparative toxicity evaluations. By synthesizing these elements, the article serves as a guide for integrating bioavailability considerations to enhance the predictive power, ethical rigor, and relevance of toxicological assessments.
Defining Bioavailability: The Critical Link Between Dose and Toxicological Effect
Core Concepts: Understanding Systemic Exposure and Site Action
What is the fundamental difference between systemic exposure and action at the site of action?
Systemic Exposure refers to the presence of a drug or compound in the systemic circulation (bloodstream), making it available throughout the body. It is typically measured by parameters such as the maximum plasma concentration (Cmax) and the area under the plasma concentration-time curve (AUC) [1] [2]. In contrast, Action at the Site of Action refers to the drug's presence and interaction with its intended biological target (e.g., a receptor, enzyme, or tissue) to produce a pharmacological or toxicological effect [3]. For most drugs, the pharmacological response is related to its concentration at this receptor site [4].
Why is it crucial to distinguish between plasma concentration and concentration at the site of action in toxicity testing?
While plasma concentrations are a convenient and standard measurement, they may not always accurately reflect the drug levels at the actual site of action (e.g., a specific organ, a tumor, or the brain) [3]. Relying solely on plasma data can be misleading because:
- Distribution Barriers: Physiological barriers, like the blood-brain barrier, can prevent a drug from reaching its target organ in the same concentration found in the plasma [3].
- Local Metabolism: Tissues may metabolize drugs differently than what is observed systemically.
- Transporters: Uptake and efflux transporters can actively pump drugs into or out of specific tissues and cells, creating a concentration gradient that differs from plasma [3].
Consequently, understanding the drug concentration at the site of action provides a more accurate basis for assessing both efficacy and toxicity [3].
How is bioavailability defined, and what factors influence it?
Bioavailability (F) is defined as the fraction of an administered dose of a drug that reaches systemic circulation unaltered [1]. An intravenously administered drug has a bioavailability of 100%. For other routes, it is calculated by comparing the AUC for that route to the AUC for an IV dose of the same drug [1].
Table 1: Key Factors Influencing Bioavailability (ADME) [5]
| Factor | Description | Impact on Bioavailability |
|---|---|---|
| Absorption | The process by which a drug enters the bloodstream from the site of administration (e.g., gut, muscle). | Affected by the drug's chemical properties, formulation, and route of administration. Low absorption reduces bioavailability. |
| Distribution | The reversible transfer of a drug from the bloodstream into tissues and organs. | A large volume of distribution may mean less drug is in the plasma, potentially reducing measurable systemic exposure for a given dose. |
| Metabolism | The chemical alteration of a drug by bodily systems, often into inactive metabolites. | Extensive first-pass metabolism in the liver or gut wall can significantly reduce the bioavailability of orally administered drugs. |
| Excretion | The removal of the drug and its metabolites from the body, primarily via kidneys or liver. | Rapid excretion can shorten the time a drug remains in systemic circulation and at the site of action. |
Additional factors include drug interactions, genetic polymorphisms in metabolizing enzymes or transporters, and pathophysiological conditions of the patient [1] [5].
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Our in vitro assay shows high efficacy, but this doesn't translate in vivo. Could this be a bioavailability issue?
Yes, this is a common challenge. High in vitro efficacy indicates that the compound is active against its target when access is unimpeded. The discrepancy in vivo often arises because the compound may not be reaching the target site in sufficient concentrations. Key areas to investigate include:
- Poor Absorption: The compound may have low permeability or solubility in the gastrointestinal tract.
- High Clearance: The compound may be rapidly metabolized (e.g., by hepatic cytochrome P450 enzymes) or excreted before it can distribute to the target tissue [1] [5].
- Efflux Transporters: Proteins like P-glycoprotein (P-gp) can actively pump the drug out of cells in the intestine or at the blood-brain barrier, limiting its absorption and tissue penetration [1] [3].
- Plasma Protein Binding: Only the unbound (free) fraction of a drug is pharmacologically active. High binding to plasma proteins like albumin can sequester the drug, reducing the amount available to diffuse into tissues [5].
FAQ 2: We are observing unexpected toxicity in a specific organ. How can we determine if it's due to localized drug accumulation?
Unexpected organ-specific toxicity can result from localized accumulation, where the drug reaches higher concentrations in a particular tissue than in the plasma. To investigate this:
- Measure Tissue Distribution: Conduct studies to directly measure drug concentrations in the affected organ versus plasma over time.
- Assess Tissue-Specific Transport: Investigate whether the organ expresses unique uptake transporters that actively concentrate the drug, or if it lacks efflux transporters that would remove it [3].
- Check for Local Metabolism: Determine if the organ metabolizes the drug into a toxic metabolite that is not formed systemically.
- Utilize PBPK Modeling: Use physiologically-based pharmacokinetic (PBPK) modeling to simulate and predict drug distribution into specific tissues and identify potential accumulation hotspots [3] [6].
FAQ 3: Our bioanalytical results are highly variable. What are common sources of error in measuring drug and metabolite concentrations?
Variability in bioanalysis can stem from multiple sources in the sample preparation and analysis workflow:
- Matrix Effects: Components in the biological sample (plasma, tissue homogenate) can suppress or enhance the ionization of the analyte in techniques like LC-MS/MS, leading to inaccurate quantification [4].
- Incomplete Sample Preparation: Inefficient extraction of the drug and metabolites from the biological matrix, whether by protein precipitation, liquid-liquid extraction, or solid-phase extraction, can cause low and variable recovery [4].
- Instability of Analytes: The drug or its metabolites may degrade during sample collection, storage, or processing if conditions (e.g., temperature, pH) are not properly controlled.
- Improper Internal Standard: Using an inappropriate internal standard that does not behave similarly to the analyte throughout the sample preparation and analysis can fail to correct for procedural variations [4].
Table 2: Troubleshooting Guide for Bioanalytical Methods
| Problem | Potential Cause | Suggested Solution |
|---|---|---|
| High variability in results | Inconsistent recovery, matrix effects, poor internal standard | Optimize extraction procedure, use a stable isotope-labeled internal standard, test for matrix effects via post-column infusion [4]. |
| Low analyte recovery | Inefficient extraction technique, analyte degradation | Re-evaluate extraction solvents and pH, ensure sample stability under processing conditions [4]. |
| Ion suppression in LC-MS/MS | Co-elution of matrix components with the analyte | Improve chromatographic separation to shift the analyte's retention time away from the "noise" region [4]. |
Experimental Protocols & Workflows
Protocol 1: Assessing Bioavailability and Systemic Exposure
Objective: To determine the absolute bioavailability of a new chemical entity (NCE) administered orally.
Methodology:
- Study Design: A crossover or parallel-group study in a relevant animal model.
- Dosing: Administer the NCE orally (PO) and intravenously (IV) at the same dose level.
- Sample Collection: Collect serial blood samples (e.g., via cannulation) at predetermined time points after both administrations.
- Bioanalysis: Process plasma samples and quantify drug concentrations using a validated bioanalytical method (e.g., LC-MS/MS) [4].
- Data Analysis: Calculate the AUC for both the PO and IV routes. Apply the formula for absolute bioavailability:
- F = (AUC~PO~ / Dose~PO~) / (AUC~IV~ / Dose~IV~) [1].
This protocol provides a direct measure of how much of the orally administered drug reaches the systemic circulation.
Protocol 2: Evaluating Drug Distribution to a Site of Action (e.g., Brain)
Objective: To evaluate the extent of drug penetration across the blood-brain barrier (BBB) into the brain.
Methodology:
- Dosing and Sampling: Administer the drug and collect paired plasma and brain tissue samples at multiple time points.
- Tissue Homogenization: Homogenize the brain tissue in a buffer.
- Drug Quantification: Analyze drug concentrations in both plasma and brain homogenate using a sensitive and specific method like LC-MS/MS [4].
- Data Analysis: Calculate the brain-to-plasma ratio (Kp) as:
- Kp = Total Drug Concentration in Brain / Total Drug Concentration in Plasma.
- For a more accurate assessment, measure the free (unbound) drug concentration in both matrices to calculate the unbound Kp (Kp,uu), which is more predictive of pharmacodynamic activity [3].
Diagram: Drug Distribution to Brain Site of Action
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Bioavailability and Distribution Studies
| Item | Function / Application |
|---|---|
| LC-MS/MS System | High-sensitivity analytical instrumentation for the quantitative determination of drugs and their metabolites in complex biological matrices like plasma, urine, and tissue homogenates [4]. |
| Stable Isotope-Labeled Internal Standards | Compounds used in bioanalysis to correct for variability and losses during sample preparation and analysis, improving accuracy and precision [4]. |
| Solid-Phase Extraction (SPE) Cartridges | Used for sample clean-up and concentration of analytes from biological fluids, helping to reduce matrix effects prior to LC-MS/MS analysis [4]. |
| Physiologically-Based Pharmacokinetic (PBPK) Modeling Software | Computational tools that simulate the absorption, distribution, metabolism, and excretion (ADME) of compounds in virtual populations, used to predict tissue exposure and extrapolate from in vitro to in vivo data [3] [6]. |
| In Vitro System for Transporter Assays | Cell-based systems (e.g., transfected cells) used to study the role of specific uptake or efflux transporters (e.g., P-gp, BCRP) on drug permeability and distribution [3]. |
| Metaflumizone-d4 | Metaflumizone-d4, MF:C24H16F6N4O2, MW:510.4 g/mol |
| 2-Deoxy-2-fluoro-D-glucose-13C | 2-Deoxy-2-fluoro-D-glucose-13C, MF:C6H11FO5, MW:183.14 g/mol |
Diagram: Predictive Workflow from In Vitro to In Vivo
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between a chemical's hazard and its risk?
The hazard of a chemical is its inherent potential to cause harm, while the risk is the likelihood that such harm will occur under specific conditions of exposure [7]. A substance may be highly hazardous, but if there is no exposure, or exposure is below a harmful level, the risk is low or nonexistent. Toxicologists quantify this relationship as: Risk = Hazard x Exposure [7].
Q2: How does bioavailability connect hazard and risk in toxicity assessments?
Bioavailability acts as a critical modifier between hazard and risk. It measures the fraction of a substance that reaches systemic circulation and is available at the site of action [1]. A high-hazard substance with low bioavailability may present a lower risk because only a small amount of the ingested dose is actually absorbed and can cause toxic effects [8]. Therefore, accurate risk assessment must account for bioavailability, not just total contaminant concentration or inherent hazard [9].
Q3: What key pharmacokinetic parameters are used to quantify bioavailability?
Bioavailability (F) is quantitatively assessed using parameters derived from plasma concentration-time profiles [1]. The table below summarizes these key parameters:
| Parameter | Symbol | Definition & Significance in Bioavailability |
|---|---|---|
| Absolute Bioavailability | F | The fraction of an administered drug that reaches the systemic circulation, compared to an intravenous (IV) dose (where F=100%) [10] [1]. |
| Area Under the Curve | AUC | The total integrated area under the plasma drug concentration-time curve. It represents the total exposure of the body to the drug over time and is directly proportional to the amount of drug absorbed [10] [1]. |
| Maximum Concentration | C~max~ | The peak plasma concentration of a drug after administration. It indicates the rate of absorption [11]. |
| Time to Maximum Concentration | T~max~ | The time it takes to reach C~max~ after drug administration. It is another indicator of the absorption rate [10]. |
Q4: How do nanoparticle carriers influence drug bioavailability and toxicity?
Nanoparticles (NPs) are used to improve the solubility and bioavailability of poorly absorbed compounds like resveratrol [11]. However, the nanocarriers themselves can introduce new toxicological considerations. A study on resveratrol-loaded nanoparticles found that the "empty" nanocarriers (without the active drug) sometimes induced higher mortality, DNA damage, and malformations than the drug-loaded nanoparticles [11]. This highlights that both the active ingredient and its delivery system must be evaluated for a complete safety assessment of nano-formulations [11].
Q5: What is the difference between bioaccessibility and bioavailability?
Bioaccessibility is the fraction of a substance that is dissolved in the gastrointestinal fluids and becomes potentially available for absorption. Bioavailability is the fraction that is actually absorbed and reaches the systemic circulation [8]. In vitro tests typically measure bioaccessibility, which can be used to predict in vivo bioavailability after proper calibration [8].
Troubleshooting Guides
Problem: Inconsistent or Low Bioavailability Readings in Animal Models
Potential Causes and Solutions:
Cause 1: Improper Study Design for Relative Bioavailability (RBA) Calculation.
- Solution: Ensure your experimental design includes the correct control groups. To calculate the Oral RBA of a test material (e.g., a lead particle), you must include groups that receive the same substance in a soluble reference form (e.g., lead acetate), both orally and intravenously (IV). The IV group is used to determine the Absolute Bioavailability (ABA) of the reference material [8]. The RBA of the test material is then calculated using the formula:
RBA = (Internal Dose Metric from oral test material / Internal Dose Metric from oral reference) x (Dose of oral reference / Dose of oral test material)[8]. - Protocol: Administer similar dose ranges of the test material and the reference material to ensure the dose-response curves are comparable. Use low to high doses to capture potential saturation in absorption [8].
- Solution: Ensure your experimental design includes the correct control groups. To calculate the Oral RBA of a test material (e.g., a lead particle), you must include groups that receive the same substance in a soluble reference form (e.g., lead acetate), both orally and intravenously (IV). The IV group is used to determine the Absolute Bioavailability (ABA) of the reference material [8]. The RBA of the test material is then calculated using the formula:
Cause 2: Overlooked Effects of the Test Formulation or Carrier.
- Solution: Always include a control group that is administered the "empty" formulation or carrier (e.g., the nanocarrier without the active compound). As demonstrated with Tween 80 and carboxymethyl chitosan nanoparticles, the carrier itself can cause toxicity, DNA damage, or estrogenic effects, which can confound the results for the active compound [11].
Cause 3: Unaccounted For Variability in Animal Gut Physiology.
- Solution: Be aware of life-span considerations. Gastric pH, intestinal absorption, and liver metabolism (first-pass effect) vary significantly in neonates and older animals compared to adults [12]. Choose an animal model whose digestive physiology best aligns with your research question and human population of interest.
Problem: High Uncertainty in Clinical Toxicology Data (e.g., Overdose Cases)
Potential Causes and Solutions:
- Cause: Missing or Unreliable Data on Dose and Timing.
- Solution: In clinical toxicology, the exact dose and time of ingestion are often unknown [13]. Implement Bayesian statistical approaches that treat the reported dose and time as random variables within defined bounds (e.g., provided by patient recall or first-responders). Use a veracity scale to weight the credibility of the patient's history, which is then incorporated into the prior distribution for dose estimation in pharmacokinetic models [13].
Experimental Protocols
Protocol 1: Determining Oral Relative Bioavailability (RBA) in an Animal Model
This protocol outlines the key steps for assessing the RBA of a substance, such as a metal or a drug, in a particulate form.
1. Objective: To determine the Oral Relative Bioavailability of a test material (TM) relative to a soluble reference material (REF).
2. Materials:
- Test Animals: Young, fasted animals (species as appropriate for the test substance).
- Test Material (TM): The substance of interest (e.g., lead-contaminated soil, drug nanoparticles).
- Reference Material (REF): A soluble form of the active compound (e.g., lead acetate for lead studies).
- Dosing Solutions: Prepared at various concentrations in an appropriate vehicle.
- Equipment: Syringes, gavage needles, microcentrifuges, analytical instrument (e.g., ICP-MS, HPLC-MS) for quantifying the internal dose metric (e.g., blood lead level, plasma drug concentration).
3. Procedure:
- Step 1: Group Allocation. Randomly assign animals to the following groups:
- Group 1 (Control): Purified diet only.
- Group 2 (Oral REF): Receives the reference material orally at multiple dose levels.
- Group 3 (IV REF): Receives the reference material intravenously (to determine absolute bioavailability).
- Group 4 (Oral TM): Receives the test material orally at multiple dose levels.
- Step 2: Dosing. Administer the substances to the animals via the appropriate route. Ensure the dose ranges for the oral REF and oral TM groups are similar and cover from low to high concentrations.
- Step 3: Sample Collection. Collect blood samples at multiple time points post-administration according to a predetermined schedule to define the concentration-time curve.
- Step 4: Sample Analysis. Process and analyze the blood samples to determine the chosen Internal Dose Metric (IDM), such as the Area Under the Curve (AUC) of concentration vs. time or the concentration in a target organ.
- Step 5: Data Analysis and RBA Calculation. Calculate the RBA using the formula [8]:
RBA = (AUC oral TM / AUC oral REF) x (Dose oral REF / Dose oral TM)
Protocol 2: In Vitro Bioaccessibility Testing for Lead Particles
This protocol is used as a faster, cheaper screening tool to estimate the potential oral bioavailability of lead in particles, calibrated against in vivo data [8].
1. Objective: To estimate the bioaccessible fraction of lead in solid samples (e.g., soil, paint, dust) using a simulated gastrointestinal extraction.
2. Materials:
- Test Sample: Homogenized, sieved soil, dust, or other solid material.
- Gastric Solution: A solution simulating stomach fluid (e.g., containing pepsin, adjusted to low pH with HCl).
- Intestinal Solution: A solution simulating small intestine fluid (e.g., containing bile salts and pancreatin, adjusted to neutral pH).
- Incubator/Shaker.
- Centrifuge and Filters (e.g., 0.45 μm).
- Analytical Instrument: Inductively Coupled Plasma Optical Emission Spectrometry (ICP-OES) or Mass Spectrometry (ICP-MS).
3. Procedure:
- Step 1: Gastric Phase. Weigh a sample into a extraction vessel. Add the gastric solution and incubate for 1 hour with continuous agitation, maintaining temperature at 37°C.
- Step 2: Intestinal Phase. After the gastric phase, adjust the pH of the mixture to the intestinal range and add the intestinal solution. Incubate for an additional 4 hours under the same conditions.
- Step 3: Separation. Centrifuge the final mixture and filter the supernatant.
- Step 4: Analysis. Analyze the filtered solution for lead concentration using ICP-OES/MS.
- Step 5: Calculation. Calculate the bioaccessible fraction as:
(Mass of Pb in extract / Total mass of Pb in the sample) x 100.
Visualizing the Concepts
Hazard vs Risk and Bioavailability
Key Pharmacokinetic Parameters
The Scientist's Toolkit: Key Research Reagents and Materials
The following table lists essential materials used in bioavailability and toxicity testing, particularly for environmental and pharmaceutical research.
| Research Reagent / Material | Function in Experiment |
|---|---|
| Carboxymethyl Chitosan (CMCS) | A polymer used as a nanocarrier to improve the solubility and delivery of poorly soluble drugs like resveratrol [11]. |
| Tween 80 | A nonionic surfactant used to stabilize nanoparticle dispersions and improve drug solubility [11]. |
| Lead Acetate (PbAc) | A readily soluble lead salt used as the reference material in in vivo experiments to determine the Relative Bioavailability (RBA) of lead from other sources (e.g., soil, paint) [8]. |
| Biochar | A carbon-rich material used in soil remediation to immobilize organic contaminants and heavy metals, thereby reducing their bioavailability and toxicity [9]. |
| Compost | An organic amendment used in soil remediation to stimulate microbial activity, enhancing the biodegradation of hydrocarbons and reducing the bioavailable fraction of contaminants [9]. |
| Activated Charcoal | Used in clinical toxicology as a decontamination agent. It adsorbs toxins in the GI tract, reducing their absorption (bioavailability) and the risk of systemic toxicity [13]. |
| N-Desmethyl Azelastine-d4-1 | N-Desmethyl Azelastine-d4-1, MF:C21H22ClN3O, MW:371.9 g/mol |
| Grp78-IN-2 | Grp78-IN-2|GRP78 Inhibitor|For Research Use |
FAQs: Core Concepts and Troubleshooting
How do solubility, lipophilicity, and molecular size collectively influence bioavailability?
These three properties are interconnected pillars that determine a drug's journey from administration to systemic circulation.
- Solubility is the prerequisite for absorption. A drug must dissolve in the gastrointestinal (GI) fluids before it can cross the intestinal wall. Drugs with aqueous solubilities less than 100 µg/mL often present dissolution-limited absorption [14].
- Lipophilicity governs permeability. It determines how easily a dissolved drug molecule can cross lipid-based biological membranes to enter the bloodstream. An optimal lipophilicity (often represented as LogP between 1 and 3) is required to balance solubility and membrane permeability [15].
- Molecular Size affects diffusion rate. Smaller molecules (typically with a molecular weight ≤ 500 Da) generally diffuse more readily through membranes than larger, bulkier compounds [15].
The Biopharmaceutics Classification System (BCS) leverages these properties to categorize drugs and predict absorption challenges [15]. A drug with poor solubility (BCS Class II or IV) will struggle to achieve sufficient concentration in the GI tract, while a drug with poor permeability (BCS Class III or IV) will have difficulty crossing the intestinal barrier.
What are the gold-standard methods for measuring these key properties?
The following table summarizes the standard experimental methods used to characterize these physicochemical drivers [16] [17] [14].
Table 1: Gold-Standard Methods for Assessing Key Physicochemical Properties
| Property | Key Measurement Methods | Typical Output | Significance for Bioavailability |
|---|---|---|---|
| Solubility | Shake-Flask Method: Equilibrium solubility determined by incubating a well-characterized solid form in a solvent (e.g., biorelevant buffer) for ~24 hours [17]. | Saturation solubility (Cs), often in µg/mL or mol·Lâ»Â¹. | Determines the maximum achievable concentration in GI fluids, driving dissolution [14]. |
| Lipophilicity | Shake-Flask Method: Partitioning between 1-octanol (modeling membranes) and a buffer (e.g., pH 7.4) is measured at equilibrium [16]. | Log P (for neutral compounds) or Log D (pH-dependent distribution coefficient). | Predicts membrane permeability and absorption potential; optimal LogP ~1-3 for oral drugs [15]. |
| Molecular Size | Calculated Descriptors: Derived from the molecular structure. | Molecular Weight (MW), Molecular Volume. | MW ≤ 500 Da is a common guideline for oral drugs; larger molecules have reduced passive diffusion [15]. |
My compound shows high solubility in the lab but low oral bioavailability in vivo. What could be the cause?
This common issue can arise from several factors beyond intrinsic solubility:
- Poor Metabolic Stability: The compound may be extensively metabolized by enzymes in the gut wall or liver during its "first-pass" metabolism, preventing it from reaching systemic circulation [10] [14].
- Efflux by Transporters: Active efflux transporters like P-glycoprotein can pump the drug back into the gut lumen after it has been absorbed into the intestinal cells [15].
- In Vivo Solubilization vs. Lab Conditions: The laboratory may use pure aqueous buffers, whereas the GI tract contains bile salts and phospholipids that form micelles. A compound might be soluble in buffer but precipitate in the gut if it does not remain solubilized within these micelles [14].
- Incorrect Solid Form: The solid form used in lab tests (e.g., an amorphous, high-energy form) might have higher solubility than the more stable crystalline form that precipitates in the GI environment [17].
Troubleshooting Checklist:
- Confirm the thermodynamic stability of the solid form used in your solubility assay.
- Assess metabolic stability in liver microsome or hepatocyte assays.
- Investigate potential for efflux using Caco-2 or transfected cell models.
- Measure solubility in fasted-state simulated intestinal fluid (FaSSIF) or fed-state simulated intestinal fluid (FeSSIF) to better mimic in vivo conditions [17].
How can I quickly diagnose the root cause of low solubility in a compound series?
A systematic "solubility diagnosis" can identify the primary molecular property responsible, guiding a targeted improvement strategy [17]. The following workflow helps pinpoint the issue:
What computational tools are available for early-stage prediction of these properties?
In silico tools are invaluable for prioritizing compounds before synthesis. SwissADME is a free, robust web tool that provides predictions for key ADME and physicochemical properties [18].
- Solubility: It uses topological methods to estimate aqueous solubility (Log S) [18].
- Lipophilicity: It offers a consensus Log P value by combining five different prediction models (iLOGP, XLOGP3, WLOGP, MLOGP, SILICOS-IT), improving accuracy [18].
- Molecular Size and Drug-likeness: It calculates molecular weight and other descriptors and features a Bioavailability Radar that provides a quick visual assessment of whether a compound's properties fall within the optimal space for oral bioavailability [18].
Detailed Experimental Protocols
Objective: To determine the equilibrium solubility of a solid drug candidate in a pharmaceutically relevant medium.
Materials:
- Well-characterized drug substance (known solid form, e.g., crystalline)
- Biorelevant buffers (e.g., pH 2.0 for gastric conditions, pH 6.5 or 7.4 for intestinal conditions)
- Thermostated shaking water bath or incubator (set to 37°C)
- Centrifuge and centrifuge tubes (or filtration setup with compatible filters)
- Analytical instrument for quantification (e.g., HPLC-UV, LC-MS/MS)
Procedure:
- Preparation: Prepare a surplus of the solid drug substance. Pre-warm the selected buffer to 37°C.
- Saturation: Add an excess of the solid drug to a known volume of buffer in a sealed vial. The amount should ensure that undissolved solid remains at equilibrium.
- Equilibration: Place the vial in the shaking incubator at 37°C for a sufficient time to reach equilibrium (typically 24-48 hours). Shaking should be sufficient to ensure proper mixing.
- Phase Separation: After equilibration, separate the saturated solution from the undissolved solid. This is critical and can be done by:
- Centrifugation: At 37°C to prevent precipitation due to temperature change.
- Filtration: Using a pre-warmed syringe and a filter that does not adsorb the drug.
- Quantification: Dilute the clear supernatant appropriately and analyze using a validated analytical method (e.g., HPLC-UV) to determine the drug concentration.
- Analysis: Calculate the saturation solubility (Cs) from the measured concentration, typically reported in µg/mL or µM.
Objective: To measure the partition coefficient of a drug between 1-octanol and a buffer, simulating its distribution between lipid membranes and aqueous physiological fluids.
Materials:
- High-purity 1-octanol (pre-saturated with buffer)
- Buffer solution (e.g., phosphate buffer pH 7.4, pre-saturated with 1-octanol)
- Thermostated shaking water bath (set to a constant temperature, e.g., 25°C or 37°C)
- Centrifuge and centrifuge tubes
- Analytical instrument for quantification (e.g., HPLC-UV)
Procedure:
- Preparation: Pre-saturate 1-octanol and buffer by mixing them together vigorously for 24 hours and allowing them to separate. Use the respective saturated phases for the experiment.
- Partitioning: Place known volumes of the octanol-saturated buffer and buffer-saturated octanol in a vial. Add a known amount of the drug compound.
- Equilibration: Seal the vial and agitate vigorously in a shaking water bath at a constant temperature for a set period (e.g., 1 hour) to reach partitioning equilibrium.
- Separation: Transfer the mixture to a centrifuge tube and centrifuge to achieve a clean separation of the two phases.
- Sampling: Carefully sample from each phase, ensuring no cross-contamination.
- Quantification: Dilute the samples as necessary and analyze the drug concentration in both the aqueous and octanol phases using HPLC-UV.
- Calculation: Calculate the partition coefficient P using the formula:
- P = [Drug]â‚’câ‚œâ‚ₙₒₗ / [Drug]ᵦᵤᶠᶠᵉᵣ
- Log P = logâ‚â‚€ (P)
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Bioavailability-Related Experiments
| Item | Function / Application | Example / Specification |
|---|---|---|
| Biorelevant Buffers | Simulate the pH and ionic strength of different GI regions (stomach, small intestine) for dissolution and solubility testing. | HCl buffer (pH 2.0), Phosphate buffers (pH 6.5, 7.4) [16]. |
| Simulated Intestinal Fluids | More advanced media containing bile salts and phospholipids to mimic the solubilizing capacity of intestinal fluids. | FaSSIF (Fasted State), FeSSIF (Fed State) [17]. |
| 1-Octanol | A model solvent for the lipid portion of biological membranes used in partition coefficient studies. | High-purity grade, pre-saturated with the aqueous buffer of choice [16]. |
| In Vitro Permeability Models | Cell-based systems used to predict intestinal absorption and efflux. | Caco-2 cell line (human colon adenocarcinoma) [15]. |
| Chromatography Columns | For analytical quantification of drug concentrations in complex samples like solubility and partition experiments. | Reversed-phase C18 columns for HPLC/LC-MS [19]. |
| In Silico Prediction Tools | Free web-based software for predicting ADME and physicochemical properties from molecular structure. | SwissADME (http://www.swissadme.ch) [18]. |
| 15-Acetyl-deoxynivalenol-13C17 | 15-Acetyl-deoxynivalenol-13C17, MF:C17H22O7, MW:355.23 g/mol | Chemical Reagent |
| Cbl-b-IN-2 | Cbl-b-IN-2 |
Core Concepts and Key Mechanisms
This section outlines the fundamental processes that govern a compound's journey from administration to reaching its site of action, which are critical for interpreting bioavailability in toxicity testing.
What are the primary mechanisms of drug absorption?
After administration, a compound must cross biological membranes to enter the systemic circulation. This occurs primarily through three mechanisms [20]:
- Passive Diffusion: The most common mechanism, where molecules move from a region of higher concentration to one of lower concentration. Lipophilic drugs typically cross membranes via lipid diffusion, governed by their lipid-aqueous partition coefficient.
- Carrier-Mediated Membrane Transport: This includes active transport (energy-dependent, can move against concentration gradients) and facilitated diffusion (carrier-mediated but follows concentration gradients). Examples include peptide transporters (PEPT1) and organic cation transporters (OCT1) [21].
- Paracellular Pathway: Small hydrophilic molecules can pass through gaps between cells via passive diffusion, although tight junctions often limit this route [22].
What is the first-pass effect and how does it reduce bioavailability?
The first-pass effect describes metabolism that occurs before a drug reaches the systemic circulation, predominantly after oral administration [23].
- Process: Orally administered drugs are absorbed from the GI tract and enter the hepatic portal vein, which carries them directly to the liver. The liver (and sometimes the gut wall) then metabolizes a significant portion of the drug before it can reach the general bloodstream [23].
- Impact: This pre-systemic metabolism substantially reduces the oral bioavailability of many drugs, meaning a smaller fraction of the administered dose becomes systemically available. Drugs like morphine, lidocaine, and glyceryl trinitrate undergo significant first-pass metabolism [23].
How do efflux transporters limit drug bioavailability?
Efflux transporters are ATP-dependent pumps that actively transport compounds back out of cells, limiting their absorption and distribution. The most well-characterized is P-glycoprotein (P-gp) [22] [20].
- Location and Function: P-gp is present in the intestinal epithelium, liver, kidney, and blood-brain barrier. In the gut, it pumps absorbed drugs back into the intestinal lumen, effectively reducing net absorption [21].
- Clinical Significance: P-gp can act as a "gatekeeper," working in concert with metabolizing enzymes like CYP3A4 to control drug access. Inhibition or induction of P-gp can lead to significant drug-drug interactions [23].
Table 1: Key Biological Barriers and Their Impact on Bioavailability
| Barrier / Mechanism | Primary Location | Impact on Bioavailability | Key Influencing Factors |
|---|---|---|---|
| Intestinal Epithelium | Gastrointestinal Tract | Limits oral absorption | Molecular size, lipophilicity, efflux transporters (P-gp), gut wall metabolism [20] [24] |
| First-Pass Metabolism | Liver, Gut Wall | Pre-systemic inactivation of drug | Hepatic extraction ratio, intestinal enzyme activity [23] |
| Blood-Brain Barrier (BBB) | Capillaries in CNS | Protects brain from xenobiotics | Tight junctions, efflux transporters (P-gp, BCRP), passive permeability [22] [25] |
Troubleshooting Guides and FAQs
FAQ 1: Why is our compound showing low oral bioavailability in in vivo models despite good solubility?
Potential Causes and Solutions:
Cause 1: Significant First-Pass Metabolism. The compound may be extensively metabolized by the liver or gut wall before entering systemic circulation [23].
- Investigation Strategy:
- Compare plasma levels after intravenous (IV) and oral (PO) administration. A much higher AUC (Area Under the Curve) after IV administration confirms a first-pass effect.
- Conduct in vitro metabolism studies using liver microsomes or hepatocytes to assess metabolic stability.
- Potential Solutions:
- Consider alternative routes of administration (e.g., sublingual, transdermal) that bypass first-pass metabolism [23].
- Explore chemical modification to create a prodrug that is less susceptible to first-pass metabolism.
- Investigation Strategy:
Cause 2: Activity of Efflux Transporters. Transporters like P-gp may be actively pumping the compound back into the gut lumen [20] [21].
- Investigation Strategy:
- Use Caco-2 cell monolayers to assess transport. A higher efflux ratio (Basolateral-to-Apical / Apical-to-Basolateral) suggests active efflux.
- Perform transport assays with and without specific P-gp inhibitors (e.g., verapamil, zosuquidar).
- Potential Solutions:
- Formulate the drug with efflux transporter inhibitors (though this requires careful consideration of drug-drug interactions).
- Chemically modify the compound to make it a poorer substrate for the efflux transporter.
- Investigation Strategy:
FAQ 2: How can we improve the predictive power of our in vitro models for blood-brain barrier penetration?
Challenges and Methodological Refinements:
- Standard In Vitro Models Lack Complexity: Simple cell monolayers (e.g., Caco-2) may not fully replicate the BBB's tight junctions and diverse transporter expression [22] [26].
- Enhanced Protocol:
- Utilize specialized brain endothelial cell lines (e.g., hCMEC/D3) or primary cells that better express BBB-specific markers.
- Measure and ensure a high Transepithelial Electrical Resistance (TEER) to confirm the integrity of tight junctions.
- Include validated markers for paracellular (e.g., lucifer yellow) and transcellular permeability.
- Incorporate Transport Studies: Assess the compound's permeability in both directions (A-to-B and B-to-A) to identify efflux transporter substrates. Use chemical inhibitors to pinpoint specific transporters involved (e.g., P-gp, BCRP) [25].
- Enhanced Protocol:
FAQ 3: Our experimental results are highly variable between assays. How can we standardize bioavailability assessment?
Strategies for Standardization:
- Characterize and Control Assay Conditions: Variability often stems from inconsistent experimental conditions [22].
- Detailed Protocol for Cell-Based Permeability Assays:
- Cell Culture: Use low-passage number cells and ensure full monolayer differentiation. For Caco-2 cells, this typically takes 21-25 days.
- Validation: Before each experiment, measure TEER and the permeability of control compounds (e.g., high-permeability metoprolol, low-permeability atenolol).
- Dosing Solution: Use fasted-state simulated intestinal fluid (FaSSIF) or fed-state (FeSSIF) to better mimic physiological conditions, as food can affect solubility and transporter activity [24].
- Incubation Conditions: Maintain physiological temperature (37°C), pH (6.5-7.4 in the small intestine), and use an oxygenated atmosphere [22].
- Detailed Protocol for Cell-Based Permeability Assays:
- Utilize Bio-relevant Media: For solubility and dissolution testing, use simulated biological fluids (e.g., Gamble's solution, artificial lysosomal fluid) that mimic the composition of the biological environment the compound will encounter [27].
Experimental Protocols and Methodologies
Protocol: Assessing Permeability and Efflux in Caco-2 Cell Monolayers
This protocol is a standard for predicting intestinal absorption and identifying efflux transporter substrates [22].
Research Reagent Solutions:
| Reagent/Material | Function |
|---|---|
| Caco-2 cells | Human colon adenocarcinoma cell line that differentiates into enterocyte-like cells. |
| Transwell plates | Permeable supports for growing cell monolayers and separate donor/receiver compartments. |
| HBSS (Hanks' Balanced Salt Solution) | Transport buffer to maintain pH and osmotic balance. |
| Lucifer Yellow | Fluorescent paracellular marker to validate monolayer integrity. |
| Specific Transporter Inhibitors | e.g., P-gp inhibitor (Verapamil), to confirm transporter involvement. |
Methodology:
- Cell Culture and Seeding: Seed Caco-2 cells at a high density on Transwell inserts. Allow 21-25 days for full differentiation and junction formation, monitoring TEER regularly.
- Experiment Pre-treatment: Before the assay, wash monolayers with transport buffer (e.g., HBSS). For inhibition studies, pre-incubate with the inhibitor for a set time.
- Bidirectional Transport Study:
- A-to-B (Apical to Basolateral): Add the test compound to the apical donor compartment and sample from the basolateral receiver compartment over time.
- B-to-A (Basolateral to Apical): Add the test compound to the basolateral donor compartment and sample from the apical receiver compartment.
- Sample Analysis: Use HPLC-MS/MS to quantify the compound concentration in all samples.
- Data Calculation:
- Calculate the Apparent Permeability (Papp) for both directions.
- Determine the Efflux Ratio: ER = Papp (B-A) / Papp (A-B). An ER > 2 suggests active efflux.
Protocol: Determining Fraction Unbound (fu) via Equilibrium Dialysis
This method determines the fraction of drug unbound to plasma proteins, which is critical for understanding active concentration [25].
Methodology:
- Setup: Use a dialysis device with two chambers separated by a semi-permeable membrane. Add drug-spiked plasma to one side (donor) and buffer to the other side (receiver).
- Incubation: Incubate the system at 37°C with gentle agitation until equilibrium is reached (typically 4-6 hours).
- Sampling and Analysis: Measure the total drug concentration in the plasma chamber and the unbound drug concentration in the buffer chamber.
- Calculation: Calculate the fraction unbound (fu) = Cbuffer / Cplasma.
Visualization of Key Pathways and Workflows
Oral Drug Absorption and First-Pass Effect
Mechanisms of Transport Across Biological Barriers
In Vitro Bioavailability Testing Workflow
Bioavailability—the proportion of a substance that enters circulation to exert biological effects—is a critical determinant in the safety assessment of chemicals and drugs. For researchers and scientists, understanding how regulatory frameworks address bioavailability is essential for designing compliant and ethical toxicity studies. This guide explores the specific requirements and emerging shifts under FIFRA (Federal Insecticide, Fungicide, and Rodenticide Act), the FDA (Food and Drug Administration), and REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals). It provides actionable troubleshooting advice to navigate this complex regulatory landscape.
Bioavailability in Key Regulatory Frameworks
Different regulatory bodies approach bioavailability assessment with distinct requirements and emphases. The table below summarizes the core focus of each framework concerning bioavailability.
| Regulatory Framework | Region | Primary Focus for Bioavailability |
|---|---|---|
| FIFRA [28] [29] | United States | Assessing risks of pesticidal substances (e.g., in Plant-Incorporated Protectants) to human health and the environment; determining if substances are "plant regulators." |
| FDA [30] [31] | United States | Ensuring drug safety and efficacy, particularly through Bioavailability (BA) and Bioequivalence (BE) studies for new drugs and generics. |
| REACH [32] [33] | European Union | Evaluating the hazardous properties of chemical substances to manage risk; bioavailability informs the extent of exposure and required risk management measures. |
FIFRA: Regulating Pesticidal Substances
The EPA regulates pesticides under FIFRA, with a specific focus on biotechnology-derived products.
- Plant-Incorporated Protectants (PIPs): PIPs are pesticidal substances produced in living plants along with the genetic material necessary for their production [29]. When assessing the risks of PIPs, the EPA evaluates their potential to affect non-target organisms and their environmental fate [29].
- Enforcement and Clarity: The regulation of plant biostimulants under FIFRA can be complex. The EPA considers a product a pesticidal "plant regulator" if its claims suggest an intended physiological action (e.g., "root stimulator") [28]. The agency has issued significant penalties for the distribution of unregistered products with such claims [28]. Researchers should note that Congress is considering the Plant Biostimulant Act of 2025, which could amend FIFRA to exclude certain biostimulants from the definition of plant regulators [28].
FDA: Ensuring Drug Safety and Efficacy
The FDA mandates rigorous assessment of a drug's journey in the body.
- Data Integrity in Studies: For bioavailability and bioequivalence studies submitted in support of drug applications, the FDA provides guidance on achieving and maintaining data integrity for both clinical and bioanalytical portions [30]. This is critical for the reliability of study results.
- The Shift to New Approach Methodologies (NAMs): In a significant move, the FDA is phasing out animal testing requirements for monoclonal antibodies (mAbs) and other drugs, favoring more human-relevant NAMs [31]. This shift is driven by the low predictivity of animal models for human immune responses to mAbs, high costs, and ethical considerations [31]. The FDA encourages the use of Microphysiological Systems (MPS or organ-on-a-chip) and in silico models to generate data for regulatory submissions [31].
REACH: Managing Chemical Risks in the EU
REACH places the burden of proof for chemical safety on industry, where bioavailability plays a key role in exposure assessment.
- The Upcoming REACH Recast: Expected in late 2025, the REACH Recast will introduce major changes [32]. Key updates include:
- Time-bound registrations: Registrations may be valid for only 10 years, requiring renewal [32].
- Mandatory dossier updates: Companies must update dossiers when new hazard data emerges [32].
- Digital Product Passports (DPPs): Compliance data will need to be shared electronically through the supply chain [32].
- Generic Risk Approach (GRA): Restrictions may be fast-tracked for hazardous substances based on their intrinsic properties alone [32].
- Bioavailability in Site-Specific Risk Assessment: Understanding bioavailability is crucial for accurate risk assessment at contaminated sites. The EPA has developed methods, including in vivo mouse models and in vitro chemical extraction tests, to determine the bioavailability of metals like arsenic and lead in soil [33]. Using these site-specific bioavailability data can significantly alter cleanup strategies and reduce remediation costs [33].
Frequently Asked Questions (FAQs) & Troubleshooting
1. We are developing a plant biostimulant product. How can we determine if it is regulated as a pesticide under FIFRA?
- Answer: The primary factor is the claims you make about the product. If your product's labeling or marketing includes claims that it functions through physiological action to alter plant behavior (e.g., "stimulates root growth," "accelerates maturation"), the EPA will likely consider it a "plant regulator" and require FIFRA registration [28]. To avoid this, ensure claims are focused on improving soil nutrient conditions without implying a direct physiological effect on the plant [28].
- Troubleshooting: If you have already made pesticidal claims, you may need to recall marketing materials and revise your product's label. Consult EPA's 2020 "Draft Guidance for Plant Regulators and Claims" for the most current interpretation [28].
2. Our company needs to comply with the new REACH Recast. What are the most urgent steps we should take?
- Answer: You should act immediately on the following [32]:
- Conduct a REACH Readiness Audit: Review all your current substance registrations and identify any with data gaps.
- Engage Your Supply Chain: Proactively communicate with suppliers to gather full material disclosure (FMD) data, especially on Substances of Very High Concern (SVHCs).
- Plan for Dossier Updates: Establish a process to monitor new scientific data and promptly update your registration dossiers.
- Prepare for Digital Systems: Begin mapping the data required for the upcoming Digital Product Passports (DPPs).
3. The FDA is moving away from animal testing. What alternative methods are acceptable for preclinical bioavailability and toxicity testing?
- Answer: The FDA is endorsing a category of tools called New Approach Methodologies (NAMs) [31]. Acceptable methods include:
- Microphysiological Systems (MPS): Also known as organ-on-a-chip, these systems use human cells to create 3D, functioning models of human organs for high-fidelity toxicity and absorption testing [31].
- In silico Models: Computational models that can simulate and predict a drug's behavior in the body [31].
- Other In Vitro Models: This includes advanced cell cultures and organoids [34] [31].
- Troubleshooting: When submitting an Investigational New Drug (IND) application, you are encouraged to submit data from NAMs in parallel with traditional animal data. The FDA recognizes that no single NAM will be 100% accurate, so a combination of complementary approaches is often best [31].
4. We have inconsistent results in our oral drug bioavailability assays. What factors should we re-examine in our experimental design?
- Answer: Inconsistent oral bioavailability often stems from these common issues [34] [19]:
- Non-Biorelevant Dissolution Media: Using simple buffers instead of biorelevant media (e.g., FaSSGF/FeSSGF or FaSSIF/FeSSIF) that mimic the fed/fasted state and contain surfactants like bile salts [34].
- Ignoring First-Pass Metabolism: The drug may be extensively metabolized in the liver or gut wall before reaching systemic circulation. In vitro liver models (e.g., MPS) can help assess this [19] [31].
- Drug Physicochemical Properties: Factors like solubility, stability in different pH environments, and particle size can dramatically affect absorption [34] [19].
- Troubleshooting: Implement a transfer dissolution model that simulates the drug's movement from the stomach (acidic pH) to the intestines (neutral pH). This can help you observe and account for pH-dependent precipitation, a common cause of poor bioavailability [34].
Essential Experimental Protocols for Bioavailability Assessment
Protocol 1: Conducting a Bioavailability Study Using the Blood Concentration Method
This is the most common direct method for assessing systemic bioavailability [19].
Workflow Overview
Steps:
- Drug Administration: Administer the test formulation to subjects (human or animal) via the route being investigated (e.g., oral) [19].
- Blood Collection: Collect blood samples at predetermined time points post-administration (e.g., 0, 0.5, 1, 2, 4, 8, 12, 24 hours). The interval and duration depend on the drug's known pharmacokinetics [19].
- Sample Processing: Centrifuge blood samples to separate plasma or serum from blood cells [19].
- Concentration Analysis: Use a sensitive and specific analytical method (e.g., LC-MS/MS) to quantify the drug concentration in each plasma sample [19].
- Data Plotting: Plot the drug concentration in plasma against time to generate a concentration-time curve [19].
- Parameter Calculation: Calculate key pharmacokinetic parameters from the curve:
- AUC (Area Under the Curve): Represents the total exposure to the drug over time.
- C~max~ (Maximum Concentration): The peak concentration observed.
- T~max~ (Time to C~max~): The time taken to reach the peak concentration [19].
Troubleshooting Tip: If you encounter high variability between subjects, ensure the study population is well-defined and controlled for factors like diet, fasting state, and genetics. A larger sample size may also be needed [19].
Protocol 2: Using In Vitro MPS (Organ-on-a-Chip) for Toxicity Screening
This protocol leverages NAMs to assess organ-specific toxicity and metabolism, providing human-relevant data [31].
Workflow Overview
Steps:
- Model Selection and Culture: Select an MPS that models your target organ (e.g., liver, kidney, heart). Seed human primary or stem cell-derived cells into the microfluidic device and culture until they form a stable, functional micro-tissue [31].
- Dosing: Introduce the test compound into the MPS at clinically relevant concentrations. The microfluidic flow allows for repeated or continuous dosing, mimicking human exposure [31].
- Real-Time Monitoring: Continuously monitor the system for functional and viability endpoints. This can include:
- Biomarker Release: Measuring organ-specific biomarkers (e.g., albumin for liver, troponin for heart) in the effluent media.
- Metabolic Activity: Using assays like ATP content.
- Morphological Changes: Using microscopic imaging [31].
- Endpoint Analysis: At the end of the experiment, analyze the system for additional endpoints, such as metabolite formation (to assess bioactivation) and transcriptomic changes [31].
- Data Integration and IVIVE: Use the collected in vitro data to perform In Vitro to In Vivo Extrapolation (IVIVE), often with the aid of computational (in silico) models, to predict human physiological responses [31].
Troubleshooting Tip: If the MPS model shows poor functionality or rapid deterioration, verify the quality of the primary cells used and ensure the microfluidic system is properly maintaining physiological shear stress and nutrient/waste exchange [31].
The Scientist's Toolkit: Key Reagents & Materials
The following table lists essential materials used in bioavailability and toxicity studies, referencing the protocols above.
| Item | Function/Brief Explanation | Example Use Case |
|---|---|---|
| Biorelevant Dissolution Media (FaSSGF, FeSSIF, etc.) [34] | Simulates the composition (pH, bile salts, lipids) of human gastric and intestinal fluids for more predictive in vitro dissolution testing. | Predicting the oral absorption of a poorly soluble drug under fasted vs. fed conditions [34]. |
| LC-MS/MS System [19] | (Liquid Chromatography with Tandem Mass Spectrometry) A highly sensitive and specific analytical instrument for quantifying low concentrations of drugs and metabolites in complex biological samples like plasma. | Measuring plasma concentration-time profiles for BA/BE studies [19]. |
| Microphysiological System (MPS) [31] | A microfluidic device that cultures living human cells in a 3D architecture to emulate the structure and function of human organs. Used for human-relevant toxicity and ADME screening. | Assessing liver toxicity or cardiotoxicity of a new drug candidate without animal testing [31]. |
| Caco-2 Cell Line [34] | A human colon adenocarcinoma cell line that, when differentiated, exhibits properties of intestinal enterocytes. Used in in vitro models to predict drug permeability and absorption. | Screening the permeability of multiple lead compounds during early drug development [34]. |
| Cryopreserved Hepatocytes [31] | Primary human or animal liver cells, preserved for storage. Used in suspension or cultured formats to study hepatic metabolism and drug-drug interactions. | Evaluating the metabolic stability and metabolite profile of a new chemical entity [31]. |
| Bet-IN-12 | Bet-IN-12, MF:C30H32FN5O2, MW:516.6 g/mol | Chemical Reagent |
| Fteaa | FTEAA|MAO Inhibitor|For Research Use |
Measuring Bioavailability: From In Vivo Models to In Vitro and In Silico Approaches
Troubleshooting Guides & FAQs
Earthworm Survival Assays: Low Dispersal or Activity Rates
Problem: Earthworms show low dispersal from assay tubes or low activity in soil quality tests, making it difficult to interpret results.
Solution: This problem often relates to suboptimal soil conditions or experimental setup. The table below outlines common issues and verified solutions based on established methodologies [35] [36].
| Problem | Possible Cause | Verified Solution |
|---|---|---|
| Low dispersal in field assays | Poor soil quality (e.g., contamination, unfavorable pH) at the target site [36]. | Use a high-quality reference soil in the assay tubes. Correlate dispersal behavior with soil physicochemical properties like metal concentration, electrical conductivity, and pH [36]. |
| Uncertain earthworm activity in lab/field | Reliance on presence alone is unreliable; worms can be inactive for long periods [35]. | Implement a density-based separation method: Place earthworms in a 1.08 g cmâ»Â³ sucrose solution. Actively feeding (active) earthworms with soil-filled guts will sink; inactive ones with empty guts will float [35]. |
| Inconsistent activity measurements | Subjective visual assessment of estivation (dormancy) [35]. | Adopt the objective density-based method, which is highly correlated with visual estimation but is applicable to a wider range of species, including those that do not estivate [35]. |
Experimental Protocol: Earthworm Dispersal Assay for Soil Quality [36] This protocol provides a rapid, in-situ technique for assessing soil quality based on earthworm preference.
- Assay Setup: Insert multiple tubes containing a standardized, preferable reference soil into the soil at your target field sites.
- Introduction of Earthworms: Place individual earthworms into the center of each assay tube.
- Monitoring and Data Collection: After a set period (e.g., 24 hours), record the behavior of each earthworm. The endpoints are:
- Dispersed: The earthworm has moved from the tube into the surrounding target soil.
- Remained: The earthworm is still within the reference soil inside the tube.
- Avoided (Escaped): The earthworm has crawled up the tube to escape both soil options.
- Died: The earthworm has died.
- Interpretation: A high rate of dispersal into the surrounding soil indicates the target soil is of high quality and preferable to the earthworms.
Rodent Models: Low Bioavailability of Oral DHA Supplements
Problem: When administering Docosahexaenoic Acid (DHA) to rodent models for toxicity or efficacy studies, the plasma concentration and bioavailability of DHA are lower than expected.
Solution: Low bioavailability is often due to DHA's poor water solubility. The following solutions, proven in rodent studies, can enhance absorption [37] [38].
| Problem | Possible Cause | Verified Solution |
|---|---|---|
| Low plasma DHA after oral gavage | Poor solubility and dispersion of standard DHA oil formulations [38]. | Co-administer DHA with a bioavailability enhancer. Alpha-tocopheryl phosphate mixture (TPM) has been shown to significantly increase DHA's ( C_{max} ) and AUC in a dose-dependent manner in rats [38]. |
| Variable DHA incorporation into target tissues (e.g., retina) | The chemical form (triglyceride vs. phospholipid) of the dietary omega-3 affects its distribution and incorporation [37]. | Select the chemical form based on the target tissue. For increased DHA and very long chain PUFA content in the retina, DHA-rich triglycerides and EPA-rich phospholipids were most effective in rat studies [37]. |
| Inconsistent tissue DHA levels | High dietary intake of linoleic acid (LA, n-6) can inversely compete with n-3 LC-PUFA incorporation, particularly in the retina [37]. | Control the dietary ratio of LA to ALA. Design experimental diets with a balanced ratio (e.g., between 4 and 5) to improve n-3 incorporation [37]. |
Experimental Protocol: Evaluating DHA Bioavailability in Rodent Models [38] This protocol outlines a method to test the effectiveness of a bioavailability enhancer (TPM) on DHA absorption in rats.
- Formulation Preparation:
- Prepare control formulation: Mix DHA oil (e.g., Incromega DHA 500TG) with a vehicle like canola oil.
- Prepare experimental formulations: Dissolve TPM powder into canola oil with mixing and mild heat (40°C). Once cooled, mix with DHA oil to achieve the desired w/w ratios (e.g., 1:0.1 and 1:0.5 DHA-to-TPM).
- Animal Dosing:
- Use male Sprague-Dawley rats (200-300 g). House under standard conditions with free access to food and water.
- Randomize rats into treatment groups (e.g., n=10). Administer formulations via oral gavage. Doses should be calculated based on body weight (e.g., a low dose of 88.6 mg DHA/kg and a high dose of 265.7 mg DHA/kg).
- Sample Collection and Analysis:
- Collect blood plasma samples at multiple time points over 24 hours post-administration.
- Analyze DHA plasma concentration using appropriate analytical methods (e.g., gas chromatography).
- Data Analysis:
- Plot DHA plasma concentration over time.
- Calculate pharmacokinetic parameters: AUC (Area Under the Curve), which represents total exposure, and ( C_{max} ), the maximum concentration. Compare these parameters between control and TPM-formulated groups to assess bioavailability enhancement.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Alpha-tocopheryl phosphate mixture (TPM) | A lipidic excipient that forms vesicles to encapsulate and solubilize poorly water-soluble nutrients like DHA, significantly improving their oral bioavailability in rodent models [38]. |
| Sucrose Solution (1.08 g cmâ»Â³) | Used for density-based separation of active and inactive earthworms. Active earthworms with soil-filled guts have a higher density and sink in this solution [35]. |
| Incromega DHA 500TG | A commercially available triglyceride-form of omega-3 oil, predominantly containing DHA, used as a standard for dosing in rodent bioavailability studies [38]. |
| Allolobophora chlorotica, Aporrectodea caliginosa | Species of endogeic earthworms (soil-feeding) commonly used in soil quality and toxicity testing assays [35]. |
| Sprague-Dawley Rats | An outbred strain of albino rat, frequently used as the rodent model in preclinical toxicology and pharmacokinetic studies, including DHA bioavailability research [38]. |
| Krill Oil | A natural source of omega-3 fatty acids (EPA and DHA) where they are present primarily in the phospholipid form, used in studies comparing the bioavailability of different chemical forms [37]. |
| rel-Biperiden-d5 | rel-Biperiden-d5, MF:C21H29NO, MW:316.5 g/mol |
| Trk-IN-16 | Trk-IN-16, MF:C19H20FN5O, MW:353.4 g/mol |
Experimental Workflow Visualizations
Earthworm Activity and Soil Quality Assessment
Enhancing DHA Bioavailability in Rodents
Technical Troubleshooting Guides
Common Experimental Challenges and Solutions
Table 1: Troubleshooting Bioaccessibility Extraction Methods
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Underestimated bioaccessibility | Insufficient sink capacity in extraction medium [39] | Implement infinite sink conditions (e.g., MEBE, Tenax, sorptive sinks); maximize acceptor-to-sample capacity ratio [39] [40]. |
| Low method reproducibility | Non-standardized assay techniques and methodology [41] | Adhere to validated protocols (e.g., UBM, SBRC); ensure within-lab repeatability (<10% RSD) and between-lab reproducibility (<20% RSD) [41]. |
| Poor correlation with in vivo bioavailability | Weak in vitro-in vivo correlation (IVIVC) [41] | Validate method against established animal models; target a linear correlation coefficient (r) > 0.8 [41]. |
| Slow desorption kinetics | Strong sorption to soil organic matter or black carbon; aging effects [39] [40] | Use a depletion-based method (e.g., sequential Tenax extraction) to measure the rapidly desorbing fraction (Frapid) [40] [42]. |
| Difficulty in analyte separation | Incomplete separation of extraction beads (e.g., Tenax) from soil matrix [39] | Use a physical membrane (e.g., LDPE in MEBE) to separate the desorption medium from the acceptor phase [39]. |
| Low analyte recovery from sink | High retention in sorptive polymers (e.g., PDMS-activated carbon) [39] | Select a sink that allows for easy back-extraction (e.g., silicone rods) or provides a directly analyzable extract (e.g., ethanol in MEBE) [39] [40]. |
Method Selection Guide
Table 2: Comparison of Key Chemical Extraction Methods for Bioaccessibility
| Method | Target Contaminants | Measured Fraction | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Membrane Enhanced Bioaccessibility Extraction (MEBE) [39] | HOCs (e.g., PAHs) | Bioaccessible | Independently controls desorption conditions and sink capacity; produces HPLC-ready extracts [39]. | Method is relatively new; requires specific equipment (LDPE membranes) [39]. |
| Tenax Extraction [40] [42] | HOCs | Rapidly Desorbing Fraction (Frapid) or 6-hour fraction (F6h) | Understands desorption kinetics; cost-effective as Tenax is reusable [40] [42]. | Time-consuming and laborious (sequential); difficult bead separation from soil [39] [40]. |
| HPCD Extraction [43] | HOCs (e.g., PAHs) | Labile/Desorbable Fraction | Rapid, easy operation; correlates well with microbial degradation [43]. | Species-dependent performance; limited extraction capacity [40]. |
| Diffusive Gradients in Thin-films (DGT) [44] [45] | Metal(loid)s (e.g., Cd, As, Pb) | Labile/Bioavailable Concentration | In-situ measurement; reflects dynamic resupply from soil solid phase; correlates well with plant uptake [44] [45]. | Not suitable for hydrophobic organic contaminants [44]. |
| Solid-Phase Microextraction (SPME) [40] [42] | HOCs | Freely Dissolved Concentration (Cfree)/Chemical Activity | In-situ application; can be deployed in various media; no solvent required [40] [42]. | Longer equilibration times for some compounds; low fiber capacity [42]. |
| Unified BARGE Method (UBM) [41] | Metal(loid)s | Bioaccessible (Gastrointestinal) | Physiologically-based; standardized for human health risk assessment [41]. | Complex protocol with multiple phases; specific to ingestion exposure pathway [41]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between bioaccessibility and bioavailability?
A1: Bioaccessibility refers to the fraction of a contaminant that is released from its matrix (e.g., soil, food) into digestive or environmental fluids and is therefore available for absorption [46] [47]. It represents the maximum potentially available pool. Bioavailability, specifically absolute bioavailability (ABA), is the fraction of the ingested contaminant that crosses the gastrointestinal barrier, enters systemic circulation, and is available for distribution to tissues [41]. In vitro bioaccessibility (IVBA) assays are often used as a surrogate to estimate the more complex and costly in vivo bioavailability [41].
Q2: When should I use a method that measures the rapidly desorbing fraction (like Tenax) versus one that measures freely dissolved concentration (like SPME)?
A2: The choice depends on the process you wish to predict.
- Use Tenax extraction (measuring bioaccessibility) for processes like biodegradation or when bioaccumulation is influenced by the ingestion of soil particles, as these are governed by the mass of contaminant that can be mobilized within a relevant time frame [40] [42].
- Use SPME (measuring freely dissolved concentration, Cfree, related to chemical activity) for predicting baseline toxicity or the passive diffusive uptake of contaminants by organisms like aquatic invertebrates, as these are driven by chemical activity gradients [40] [42]. Both methods have been successfully correlated to bioaccumulation in various scenarios.
Q3: My research involves metals in soils. Which method is most reliable for predicting plant uptake?
A3: Recent studies indicate that the Diffusive Gradients in Thin-films (DGT) technique often shows a superior correlation with plant uptake of metals like Cd compared to traditional chemical extraction methods (e.g., CaClâ‚‚, DTPA, HAc) [44] [45]. This is because DGT mimics the dynamic root uptake by creating a sink for metal ions, considering both the soil solution concentration and the resupply from the solid phase [45]. For direct human health risk assessment via ingestion, physiologically-based extraction methods like the Unified BARGE Method (UBM) are more appropriate [41].
Q4: How can I validate that my in vitro bioaccessibility results are meaningful for in vivo scenarios?
A4: Validation involves establishing a strong correlation between your in vitro measurements and results from in vivo bioavailability studies. According to expert recommendations, a robust model should demonstrate [41]:
- A linear relationship with a correlation coefficient (r) > 0.8.
- A slope of the regression line between 0.8 and 1.2.
- Acceptable precision, with within-lab repeatability of < 10% relative standard deviation (RSD) and between-lab reproducibility of < 20% RSD.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Bioaccessibility assays
| Item | Function/Application | Example Use Case |
|---|---|---|
| 2-Hydropropyl-β-Cyclodextrin (HPCD) | Acts as a mild solubilizing agent that can form inclusion complexes with HOCs, mimicking desorption into aqueous phases [39] [43]. | HPCD shake extraction to predict the microbial bioaccessibility of PAHs in soil [43]. |
| Tenax Beads | A porous polymer used as a sorptive sink to continuously remove HOCs desorbed from soil, allowing measurement of the rapidly desorbing fraction [40]. | Sequential or single-point (e.g., 6-hour) Tenax extraction to estimate the bioaccessible fraction of PCBs in sediments [40] [42]. |
| Low-Density Polyethylene (LDPE) Membrane | A semipermeable membrane that physically separates a mild aqueous desorption medium from an organic acceptor solvent, creating a defined and infinite sink [39]. | Used in the MEBE setup to extract PAHs from soil with independent control over desorption conditions and sink capacity [39]. |
| SPME Fibers | Coated fibers that absorb HOCs until equilibrium is reached with the freely dissolved concentration (Cfree) in the sample, used to measure chemical activity [40] [42]. | Deploying PDMS-coated fibers in water or sediment suspensions to predict the bioavailability of pesticides to benthic organisms [42]. |
| Polyoxymethylene (POM) Sampler | A passive equilibrium sampler used to measure the freely dissolved concentration (Cfree) of HOCs in sediment or soil [40]. | Determining Cfree of PAHs in sediment porewater for use in equilibrium partitioning models [40]. |
| Enzymes & Bile Salts | Key components of physiologically-based extraction tests that simulate the solubilizing and digestive conditions of the human gastrointestinal tract [41]. | Incorporated into the Unified BARGE Method (UBM) to assess the human bioaccessibility of arsenic in contaminated soils [41]. |
| Egfr-IN-69 | Egfr-IN-69, MF:C31H37Cl2N7O3S, MW:658.6 g/mol | Chemical Reagent |
| Akr1C3-IN-6 | Akr1C3-IN-6|Potent AKR1C3 Inhibitor|For Research Use | Akr1C3-IN-6 is a potent and selective AKR1C3 inhibitor for cancer research. It targets castration-resistant prostate cancer (CRPC) mechanisms. This product is For Research Use Only. Not for human or veterinary use. |
Conceptual Framework and Experimental Workflows
Conceptual Framework for Bioavailability and Bioaccessibility
The following diagram illustrates the key concepts and their relationships in assessing contaminant fate and effects.
Generalized Workflow for a Bioaccessibility Experiment
This workflow outlines the common steps for conducting and validating a bioaccessibility study, from sample preparation to data interpretation.
Frequently Asked Questions (FAQs)
Q1: What is the core practical difference between linear and log-linear trapezoidal methods for calculating AUC?
The choice primarily affects accuracy in different phases of drug disposition. The linear trapezoidal method uses linear interpolation between all concentration-time points and is simple to implement but can overestimate AUC during the elimination phase because it does not account for the exponential (first-order) nature of drug elimination. In contrast, the logarithmic trapezoidal method uses logarithmic interpolation and is more accurate for decreasing concentrations. For the most accurate overall result, a hybrid approach is recommended: use the linear method for rising concentrations (absorption phase) and the logarithmic method for declining concentrations (elimination phase). This hybrid is often called "Linear-Up Log-Down." The impact of the method is more pronounced with widely spaced time points [48].
Q2: My PK model fails to converge. Could poor initial parameter estimates be the problem?
Yes, this is a common issue. Nonlinear mixed-effects models, which are central to population PK (PopPK) analysis, rely on adequate initial parameter estimates for efficient optimization. Poor initial estimates can lead to failed convergence or incorrect final parameter estimates. This is especially problematic with sparse data, where traditional methods like non-compartmental analysis (NCA) struggle. Automated pipelines that use data-driven methods (e.g., adaptive single-point methods, graphic methods, and parameter sweeping) are now being developed to generate robust initial estimates for parameters like clearance (CL) and volume of distribution (Vd), thereby improving model convergence and reliability [49].
Q3: When is a suprabioavailable product a regulatory concern, and what are the next steps?
A suprabioavailable product displays an appreciably larger extent of absorption than the approved reference product. This is a regulatory concern because it could lead to higher systemic exposure and potential toxicity if patients are switched to the new product without dose adjustment. If suprabioavailability is found, the developer should consider formulating a lower dosage strength. A comparative bioavailability study comparing the reformulated product with the reference product must then be submitted. If a lower strength is not developed, the dosage recommendations for the suprabioavailable product must be directly supported by clinical safety and efficacy studies [50].
Q4: What is the role of Incurred Sample Reanalysis (ISR) in a bioanalytical study?
ISR is a regulatory requirement (e.g., in the EMA Guideline on Bioanalytical Method Validation) to confirm the reliability and reproducibility of the analytical method used to generate PK data. It involves reanalyzing a portion of study samples in a separate analytical run to verify that the original concentration data are valid. ISR helps identify issues not always caught during method validation, such as metabolite back-conversion, sample matrix effects, or analyte instability. A lack of ISR data requires a strong scientific justification, especially for pivotal studies like bioequivalence trials, as it calls into question the validity of the entire dataset [50].
Troubleshooting Guides
Troubleshooting Model Convergence Failures in PopPK Analysis
Failed model convergence often stems from inadequate initial parameter estimates. The following workflow outlines a systematic approach to diagnose and resolve this issue.
Table: Strategies for Generating Initial Parameter Estimates
| Scenario | Problem | Recommended Method | Key Action |
|---|---|---|---|
| Data-Rich | NCA may be reliable, but model initial estimates are needed. | Naïve Pooled NCA, Graphic Methods [49] | Pool all individual data or use plots to estimate primary parameters. |
| Sparse Data | NCA is unreliable or impossible; no robust starting points. | Adaptive Single-Point Method, Parameter Sweeping [49] | Use population-level summarization or test a range of values via simulation. |
| Complex Models | Multi-compartment models or nonlinear elimination. | Parameter Sweeping [49] | Simulate concentrations for candidate parameter values and select the best fit. |
Protocol: Parameter Sweeping for Complex Models [49]
- Define the Range: Establish a biologically plausible range for each parameter that lacks an initial estimate (e.g., absorption rate constant
Ka). - Generate Candidates: Create a set of candidate parameter values, often by sampling across the defined range.
- Simulate & Compare: For each candidate set, simulate the model to predict concentrations.
- Evaluate Performance: Calculate the relative Root Mean Squared Error (rRMSE) between the simulated and observed concentrations.
- Select Estimates: Choose the parameter values from the candidate set that yield the lowest rRMSE as the new initial estimates for the full PopPK model fitting.
Troubleshooting Inaccurate AUC Calculations
Inaccurate AUC determination can compromise entire pharmacokinetic studies. The following guide helps identify and correct the root cause.
Table: AUC Calculation Methods and Applications
| Method | Best Used For | Advantage | Disadvantage |
|---|---|---|---|
| Linear Trapezoidal | Absorption phase; rising concentrations [48]. | Simple to implement and compute. | Overestimates AUC during the exponential elimination phase [48]. |
| Log-Trapezoidal | Elimination phase; decreasing concentrations [48]. | More accurate for first-order elimination. | Underestimates AUC during the absorption phase. |
| Linear-Up Log-Down | General purpose, recommended as the most accurate for most studies [48]. | Applies the optimal method for each phase of the concentration-time profile. | More complex implementation than a single method. |
Protocol: Implementing a Linear-Up Log-Down AUC Analysis [48]
- Data Preparation: Ensure concentration-time data is ordered chronologically.
- Identify Phases: For each interval between consecutive time points, determine if the concentration is increasing (absorption/distribution) or decreasing (elimination).
- Apply Linear Rule: For intervals with rising concentrations, calculate the partial AUC using the linear trapezoidal formula:
AUC = (C1 + C2)/2 * (t2 - t1). - Apply Log Rule: For intervals with decreasing concentrations, calculate the partial AUC using the log trapezoidal formula:
AUC = (C1 - C2) * (t2 - t1) / ln(C1 / C2), providedC1 > C2and both are positive. - Sum Partial AUCs: The total AUC from time zero to the last measurement (
AUC0-t) is the sum of all partial AUCs.
The Scientist's Toolkit
Table: Essential Reagents, Software, and Tools for PK Analysis
| Item Name | Function / Application | Key Features |
|---|---|---|
| PKSolver | A free, menu-driven add-in for Microsoft Excel for basic PK/PD data analysis [51]. | Performs noncompartmental analysis (NCA), compartmental modeling, and provides a library of PK functions; useful for routine analysis [51]. |
| R/babelmixr2 | An R package for population PK model development that can connect with NCA tools [49]. | Integrates NCA results from tools like PKNCA to help generate initial parameter estimates for nonlinear mixed-effects modeling with nlmixr2 [49]. |
| Phoenix WinNonlin | Industry-standard software for PK/PD data analysis [48]. | Provides robust NCA capabilities, including multiple AUC calculation methods (Linear, Log, Linear-Up Log-Down) and advanced modeling features [48]. |
| Automated IE Pipeline | A data-driven approach (e.g., via a custom R package) to generate initial parameter estimates for PopPK models [49]. | Uses adaptive single-point methods, graphic methods, and parameter sweeping to create robust starting values, especially for sparse data [49]. |
| ISR (Incurred Sample Reanalysis) | A quality control process, not a physical tool, but critical for bioanalytical method validation [50]. | Reanalysis of a subset of study samples to confirm the reproducibility and reliability of the bioanalytical method used to generate concentration data [50]. |
| AChE-IN-15 | AChE-IN-15|Acetylcholinesterase Inhibitor | AChE-IN-15 is a potent acetylcholinesterase inhibitor for neurological research. This product is for research use only and not for human consumption. |
| PI3K-IN-26 | PI3K-IN-26|Potent PI3K Inhibitor for Cancer Research | PI3K-IN-26 is a potent PI3K pathway inhibitor for research into cancer mechanisms and therapy resistance. This product is For Research Use Only and is not intended for diagnostic or therapeutic use. |
Frequently Asked Questions (FAQs) on Nanotoxicology and Bioavailability
1. What is the fundamental relationship between a nanoparticle's bioavailability and its toxicity? Bioavailability—the extent and rate at which a nanoparticle enters systemic circulation or reaches a target site—is a primary determinant of its toxic potential. Even highly reactive nanoparticles cannot induce toxicity if they are not bioavailable. Key physicochemical properties such as size, surface charge, and chemical composition directly govern bioavailability by influencing how easily a particle can cross biological barriers, its distribution within tissues, and its persistence in the body [52] [53]. For instance, smaller particles typically have higher cellular uptake, and a positive surface charge often leads to stronger electrostatic interactions with negatively charged cell membranes, increasing bioavailability and potential cytotoxic effects [52].
2. Which physicochemical properties of nanoparticles are most critical to characterize in a toxicity assessment? A robust toxicity assessment requires the characterization of a core set of physicochemical properties, as these dictate both bioavailability and the mechanism of toxic action. The table below summarizes the key properties and their toxicological significance.
Table 1: Key Physicochemical Properties and Their Role in Nanotoxicity
| Property | Toxicological Influence | Experimental Consideration |
|---|---|---|
| Size | Governs cellular uptake, tissue penetration, and clearance. Smaller particles (< 20 nm) can enter cells more easily and may reach sensitive cellular compartments [52]. | Use dynamic light scattering (DLS) for hydrodynamic size and TEM/SEM for primary particle size. |
| Surface Charge | Influences interaction with cell membranes (positively charged particles often show higher uptake and toxicity) and protein corona formation [52] [53]. | Measure zeta potential in relevant biological fluids (e.g., cell culture medium). |
| Shape & Aspect Ratio | Affects cellular internalization kinetics and macrophage clearance. High-aspect-ratio materials (e.g., nanotubes) can induce frustrated phagocytosis [52]. | Characterize using electron microscopy. |
| Chemical Composition | Determines intrinsic reactivity (e.g., metal ion leaching, ROS generation) and degradation products [54] [52]. | Use ICP-MS for dissolution studies and elemental analysis. |
| Surface Area | A higher surface area provides more reactive sites, which can amplify oxidative stress and catalytic activity [52]. | Calculate from particle size and morphology or use BET analysis. |
| Agglomeration State | Alters the effective particle size and bioavailability in biological media [55] [56]. | Characterize using DLS and compare the size in water versus cell culture medium. |
3. What are the primary molecular mechanisms by which bioavailable nanoparticles induce toxicity? Bioavailable nanoparticles can trigger toxicity through several interconnected mechanistic pathways, with oxidative stress being a central player. The diagram below illustrates the core cellular events following nanoparticle exposure.
The key mechanisms include:
- Oxidative Stress: Nanoparticles can directly generate reactive oxygen species (ROS) or deplete antioxidant defenses (e.g., glutathione), leading to lipid peroxidation, protein denaturation, and DNA damage [54] [52] [53].
- Inflammation: The induction of oxidative stress often activates inflammatory signaling pathways (e.g., NF-κB), resulting in the release of pro-inflammatory cytokines such as IL-6, IL-8, and TNF-α [54] [52].
- Genotoxicity: As shown in subway nanoparticle studies, certain nanoparticles can directly cause DNA strand breaks, posing a risk for mutagenesis and carcinogenesis [55].
- Organelle Dysfunction: Nanoparticles can localize in and damage mitochondria, leading to impaired energy metabolism and the initiation of apoptosis [54] [52].
4. My in vitro assays show low cytotoxicity, but in vivo studies suggest organ toxicity. How can I resolve this discrepancy? This common issue often arises because traditional cytotoxicity assays (e.g., MTT, LDH) capture only acute cell death and overlook subtle molecular perturbations and organ-specific accumulation. To bridge this gap:
- Adopt Advanced In Vitro Models: Move beyond 2D monocultures to 3D organoids or co-culture systems that better mimic tissue complexity and barrier functions [52].
- Incorporate Omics Technologies: Implement "nanotoxicomics"—the integration of transcriptomics, proteomics, and metabolomics. This approach can identify early biomarkers of stress (e.g., changes in heat shock proteins, metallothioneins, or metabolic pathways like glutathione synthesis) long before cell death occurs [54].
- Investigate Chronic, Low-Dose Exposure: Design studies that reflect realistic exposure scenarios rather than just short-term, high-concentration challenges [57] [58].
5. How can I accurately quantify nanoparticle uptake and distribution in cells and tissues? Quantifying bioavailability requires a combination of techniques:
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS): This is the gold standard for the sensitive and quantitative measurement of metal-based nanoparticles in cells, tissues, and biological fluids [54].
- Advanced Imaging: Techniques like high-resolution TEM can visualize intracellular nanoparticles, while newer AI-powered 3D imaging ecosystems (e.g., LungVis 1.0) can profile the spatial distribution and migration of nanoparticles within entire organs, such as the lung [58].
- Single-Cell Analysis: To account for high cell-to-cell variability in nanoparticle uptake, use flow cytometry or image-based single-cell analysis to measure the nanoparticle content in individual cells [58].
Troubleshooting Common Experimental Challenges
Problem 1: Inconsistent or Irreproducible Toxicity Results Between Experimental Replicates
- Potential Cause: Dynamic transformation of nanoparticles in the biological medium. Nanoparticles can agglomerate, dissolve, or form a protein corona, changing their biological identity and bioavailability.
- Solution:
- Characterize nanoparticles in the exposure medium: Do not rely on characterization in water alone. Perform DLS and zeta potential measurements in the exact cell culture or serum-containing medium used in your experiments immediately before and during exposure [56] [52].
- Standardize dispersion protocols: Use a consistent method (e.g., sonication energy and time) to prepare nanoparticle suspensions.
- Measure actual exposure doses: Techniques like ICP-MS can verify the actual concentration of nanoparticles in contact with cells, which may differ from the nominal concentration due to agglomeration and sedimentation [54].
Problem 2: Difficulty in Differentiating Toxicity from the Nanoparticle Core Versus Leached Ions
- Potential Cause: Many metal and metal oxide nanoparticles (e.g., Ag, CuO, ZnO) undergo dissolution, releasing toxic ions that can be the primary driver of toxicity.
- Solution:
- Perform ion control experiments: Include a parallel set of experiments where you expose your models to concentrations of dissolved metal salts (e.g., AgNO₃ for AgNPs) equivalent to the amount of ions leached from the nanoparticles.
- Measure dissolution kinetics: Use ultrafiltration or dialysis coupled with ICP-MS to quantify the rate and extent of ion release from your nanoparticles in the relevant biological medium [56].
- Use particle-specific assays: Certain responses, like frustrated phagocytosis of high-aspect-ratio particles, are unique to the particulate form.
Problem 3: Low Predictive Value of In Vitro Data for In Vivo Outcomes
- Potential Cause: Oversimplified in vitro models that lack key features of in vivo systems, such as physiological barriers, immune cells, and tissue-level organization.
- Solution:
- Utilize complex co-culture models: Incorporate immune cells (e.g., macrophages) with your primary target cells to better model inflammatory cascades [55].
- Incorporate fluid flow and shear stress: Use systems that provide dynamic flow to simulate blood or air flow, which affects nanoparticle deposition and uptake.
- Leverage in silico prediction tools: Machine learning models are now being developed that integrate nanoparticle properties and in vitro data to predict in vivo outcomes like lung fibrosis with high accuracy [58] [53].
Essential Experimental Protocols
Protocol 1: A Tiered Strategy for Assessing Bioavailability and Toxicity This workflow integrates physicochemical characterization with increasingly complex biological models to thoroughly evaluate nanotoxicity.
Tier 1: Comprehensive Physicochemical Characterization
- Objective: Establish the baseline properties of the nanoparticle suspension.
- Methodology:
- Size & Agglomeration: Analyze the nanoparticle suspension in both deionized water and complete cell culture medium using Dynamic Light Scattering (DLS).
- Surface Charge: Measure zeta potential in both solvents.
- Morphology: Image particles using Transmission Electron Microscopy (TEM).
- Composition & Purity: Use techniques like ICP-MS or EDX to confirm chemical composition and detect impurities.
Tier 2: High-Throughput In Vitro Screening
- Objective: Identify overt cytotoxicity and acute toxicological triggers.
- Methodology:
- Dose-Response Cytotoxicity: Expose relevant cell lines (e.g., A549 lung epithelial cells, THP-1 macrophages, HepG2 liver cells) to a range of nanoparticle concentrations (e.g., 1-200 µg/mL) for 24-72 hours. Assess viability using metabolic (MTT/WST-1) and membrane integrity (LDH) assays [54] [52].
- Oxidative Stress: Use fluorescent probes like DCFH-DA to measure intracellular ROS levels after 2-6 hours of exposure [55] [52].
- Genotoxicity: Perform a comet assay to detect DNA strand breaks in cells after 24-hour exposure [55].
Tier 3: Advanced In Vitro Modeling
- Objective: Improve physiological relevance.
- Methodology:
- Co-culture Models: Culture target epithelial cells (e.g., A549) on a transwell insert and immune cells (e.g., dTHP-1 macrophages) in the lower chamber. Expose the system to nanoparticles and collect media from both compartments to analyze cytokine cross-talk (e.g., IL-8, IL-6, TNF-α) using ELISA [55].
- 3D Organoids: Utilize commercially available or lab-grown 3D organoid models of liver, lung, or intestine to assess toxicity in a tissue-like context with multiple cell types [52].
Tier 4: Mechanistic Omics Analysis (Nanotoxicomics)
- Objective: Uncover sub-toxic and mechanism-level effects.
- Methodology:
- Transcriptomics: Perform RNA sequencing on exposed cells to identify differentially expressed genes related to oxidative stress (e.g., HMOX1), inflammation (e.g., IL-6), and DNA damage response (e.g., TP53) [54].
- Proteomics: Use mass spectrometry to validate protein-level changes, such as the upregulation of heat shock proteins (HSPs) or metallothioneins [54].
- Metabolomics: Analyze the cellular metabolome to detect functional readouts like ATP depletion, glutathione redox state shifts, and prostaglandin E2 (PGE2) levels [54].
Protocol 2: Differentiating Particulate vs. Ionic Toxicity
- Objective: Decouple the toxic effects of the nanoparticle itself from those of its dissolved ions.
- Methodology:
- Leachate Preparation: Incubate the nanoparticle suspension in the exposure medium under the same conditions as your biological experiments (e.g., 37°C, with shaking). After 24 hours, centrifuge the suspension at high speed (e.g., 100,000 x g) to pellet the particles. Carefully collect the supernatant, which is the "leachate" containing dissolved ions [56].
- Parallel Exposure: Treat cells with three conditions:
- The complete nanoparticle suspension.
- The leachate (ion fraction).
- A solution of metal salt (e.g., AgNO₃ for AgNPs) at a concentration matched to the ion content in the leachate (measured by ICP-MS).
- Comparative Analysis: Assess all three conditions using your Tier 2 assays (cytotoxicity, ROS). If the leachate and metal salt cause similar toxicity to the whole nanoparticle, ionic release is likely the primary mechanism. If the nanoparticle is more toxic, a particulate effect is indicated.
The Scientist's Toolkit: Key Reagent Solutions
Table 2: Essential Research Reagents for Nanotoxicology Studies
| Reagent / Assay Kit | Function in Nanotoxicity Research | Key Application Notes |
|---|---|---|
| DCFH-DA Assay Kit | Measures intracellular levels of Reactive Oxygen Species (ROS). | A foundational assay for detecting oxidative stress, a primary mechanism of nanotoxicity [52]. |
| Comet Assay Kit | Detects DNA strand breaks at the single-cell level. | Critical for assessing the genotoxic potential of nanoparticles, as demonstrated in subway nanoparticle studies [55]. |
| ELISA Kits for Cytokines (IL-8, IL-6, TNF-α) | Quantifies the release of pro-inflammatory cytokines from cells. | Used to evaluate the inflammatory response in macrophage co-culture models [55] [54]. |
| Cell Viability Assays (MTT, WST-1) | Measures metabolic activity as an indicator of cell health. | Standard for initial cytotoxicity screening; use in a dose-response manner [52]. |
| Lactate Dehydrogenase (LDH) Assay Kit | Measures cell membrane damage (necrosis). | Complements metabolic assays by quantifying a different cell death pathway [52]. |
| ICP-MS Standard Solutions | Enables calibration for quantitative analysis of metal nanoparticle uptake and dissolution. | Essential for obtaining absolute mass-based data on bioavailability and biodistribution [54]. |
| Differentiated THP-1 Macrophages | A human monocyte cell line that can be differentiated into macrophage-like cells. | A widely used model for studying the immune cell response to nanoparticles and phagocytosis [55]. |
| 3D Organoid Culture Systems | Provides a more physiologically relevant in vitro model with multiple cell types. | Improves the in vivo predictability of toxicity findings for organs like liver, lung, and gut [52]. |
| Hbv-IN-22 | Hbv-IN-22, MF:C26H29N3O2S2, MW:479.7 g/mol | Chemical Reagent |
Troubleshooting Guides
Troubleshooting AI/ML Model Performance
Problem 1: Poor Model Performance on New Chemical Series
- Symptoms: High prediction errors (e.g., high Mean Absolute Error) for new compound classes not well-represented in training data.
- Solution:
- Implement Time-Based Splits: Evaluate model performance using a temporal split (data up to a certain date for training, newer data for testing) rather than random splits, to better simulate real-world usage and avoid over-optimistic performance metrics [59].
- Adopt a Fine-Tuned Global Model: Train models using a combination of large, curated global datasets and your specific program's local data. This approach has been shown to outperform models using only global or only local data [59].
- Retrain Models Frequently: Establish a schedule for weekly or monthly model retraining to incorporate new experimental data. This allows the model to rapidly learn from new chemical space and adjust to "activity cliffs" [59].
Problem 2: Low User Trust and Adoption of ML Predictions
- Symptoms: Medicinal chemists are hesitant to use model predictions to guide compound design.
- Solution:
- Stratify Evaluation Metrics: Proactively measure and report model performance for specific projects and chemical series. This transparent communication informs teams where models can be used confidently [59].
- Integrate Explainable AI (XAI): Use tools like SHapley Additive exPlanations (SHAP) to provide post-hoc explanations for model predictions. This reveals which molecular features (e.g., logP, TPSA) most influenced a prediction, building trust and providing chemists with actionable insights [60].
Problem 3: Model Applicability to Novel Drug Modalities
- Symptoms: Unreliable predictions for complex molecules like Targeted Protein Degraders (TPDs), which often have molecular weights beyond the Rule of 5 (bRo5).
- Solution:
- Validate on Relevant Modalities: Actively test the performance of global models on sub-modalities like heterobifunctional degraders and molecular glues. Evidence shows that while errors may be slightly higher for heterobifunctionals, global models can still provide valuable predictions, with misclassification errors for key ADME endpoints often below 15% [61].
- Apply Transfer Learning: Use transfer learning techniques to refine general models with TPD-specific data, which can improve prediction accuracy for these complex molecules [61].
Troubleshooting PBPK Modeling
Problem 1: Predicting Pharmacokinetics in Specific Populations
- Symptoms: Need to predict ADME in populations where clinical trials are ethically or practically challenging (e.g., pregnant women, pediatric patients, those with organ impairment).
- Solution:
- Leverage Population-Specific PBPK Models: Utilize PBPK models that incorporate physiological and pathophysiological changes specific to the population of interest. These models can simulate variations in drug metabolism due to age, genetics, or disease state, aiding in personalized dosing strategy and clinical trial optimization [62].
- Incorporate Genetic Polymorphism Data: Integrate data on genetic variations (e.g., in CYP enzymes) into the PBPK model to predict their impact on drug metabolism and exposure [62].
Problem 2: Inaccurate Prediction of Human PK from Preclinical Data
- Symptoms: Disconnect between predicted and observed human pharmacokinetics during lead optimization.
- Solution:
- Use PBPK for Compound Screening: Employ generic PBPK models during lead identification and optimization to provide reliable human PK predictions from early in vitro ADME data, enabling better compound selection [63].
- Integrate Machine Learning: Combine PBPK with ML-based QSAR/QSPR models that predict complex in vivo properties from structural features and in vitro data to enhance the overall prediction framework [63].
Frequently Asked Questions (FAQs)
Q1: What are the most critical best practices for successfully implementing ML models for ADME prediction in a drug discovery program? A1: The key best practices are: 1) Regular, time-based validation to build trust and ensure realistic performance estimates [59]. 2) Frequent model retraining (e.g., weekly) to continuously integrate new data and adapt to shifting chemical space [59]. 3) Combining global and local data for model training to balance broad knowledge with project-specific patterns [59]. 4) Ensuring models are interactive, interpretable, and integrated into chemists' existing design tools to facilitate use and impact [59].
Q2: Can AI/ML models accurately predict ADME properties for complex new modalities like targeted protein degraders? A2: Yes, recent comprehensive evaluations demonstrate that ML-based QSPR models show promising performance for TPDs. While prediction errors for heterobifunctional degraders can be higher than for traditional small molecules or molecular glues, the misclassification rates into high/low-risk categories for critical properties like permeability and metabolic clearance are often acceptably low (e.g., below 15%). This supports the use of ML to guide the design of TPDs [61].
Q3: How can PBPK modeling address challenges related to bioavailability and toxicity in specific populations? A3: PBPK models are particularly valuable for simulating drug disposition in populations where clinical trials are difficult. They can incorporate physiological changes associated with age (pediatrics/geriatrics), pregnancy, or organ impairment (liver/kidney disease) to predict alterations in ADME processes. This helps in assessing potential changes in bioavailability and toxicity risks, optimizing clinical trials, and informing dosing strategies for these specific groups before clinical data is widely available [62].
Q4: What role does explainable AI (XAI) play in ADME prediction? A4: XAI moves beyond the "black box" by providing insights into which molecular features drive a specific ADME prediction. Techniques like SHAP analysis can quantify the impact of descriptors like lipophilicity (logP) or polar surface area (TPSA) on predicted outcomes such as metabolic stability [60]. This transparency helps medicinal chemists understand the model's reasoning, builds trust, and provides actionable guidance for molecular design to improve ADME properties.
Q5: What is the evidence that AI is actually accelerating drug discovery? A5: There are concrete examples of accelerated timelines. For instance, Insilico Medicine progressed an idiopathic pulmonary fibrosis drug candidate from target discovery to Phase I trials in approximately 18 months, a fraction of the typical 5-year timeline for early-stage discovery [64] [65]. Furthermore, companies like Exscientia have reported designing clinical compounds using AI that require significantly fewer synthesized compounds and shorter design cycles compared to industry norms [64].
The table below summarizes key performance metrics for ML models in ADME prediction, as found in the literature.
Table 1: Performance Metrics of Machine Learning Models for ADME Prediction
| Property / Endpoint | Model Type | Performance Metric | Value (All Modalities) | Value (TPD - Heterobifunctionals) | Citation |
|---|---|---|---|---|---|
| Human Liver Microsomal (HLM) Stability | Fine-Tuned Global Model (Graph Neural Network) | Mean Absolute Error (MAE) | ~0.20 (log scale) | ~0.39 (log scale) | [61] |
| Lipophilicity (LogD) | Fine-Tuned Global Model (Graph Neural Network) | Mean Absolute Error (MAE) | 0.33 | 0.45 | [61] |
| CYP3A4 Inhibition & Microsomal Clearance | Global Multi-task Model | Misclassification Error | 0.8% - 8.1% | < 15% | [61] |
| General ADME Endpoints | Global Model vs. Local (AutoML) Model | Relative Performance | Fine-tuned global model generally achieved lower MAE than local-only models across HLM, RLM, and MDCK assays. | N/A | [59] |
Experimental Protocol: Implementing a Retrainable ML Model for ADME Optimization
This protocol outlines the steps for building and deploying a machine learning model to predict metabolic stability (e.g., HLM clearance) to guide lead optimization.
Objective: To create a predictive HLM stability model that is regularly updated with new project data to assist medicinal chemists in compound design.
Materials & Reagents:
- Software: Access to a modeling platform (e.g., Python with Deep Learning libraries like PyTorch/TensorFlow, or commercial QSAR software).
- Data: A curated historical dataset of chemical structures and corresponding HLM intrinsic clearance measurements (e.g., from an internal database or public sources like [60]).
- New Compounds: Structures and assay results for newly synthesized compounds from the ongoing project.
Procedure:
- Initial Model Training (Week 0):
- Data Preparation: Combine a large, global dataset of HLM measurements with any existing project-specific data. Apply necessary cleaning and standardization.
- Train-Test Split: Perform a time-based split, reserving the most recent 10-20% of compounds (by synthesis date) as a test set [59].
- Model Training: Train a graph neural network or random forest model on the training set. Use cross-validation to tune hyperparameters.
- Initial Validation: Evaluate the model on the held-out test set and report metrics (MAE, Spearman R) for the overall set and for key chemical series [59].
Deployment and Weekly Update Cycle:
- Integration: Deploy the model as an interactive tool within the chemists' design software, allowing for real-time prediction of new, virtual compounds [59].
- Weekly Retraining: a. Data Incorporation: Each week, add the new HLM data from compounds synthesized and tested in the previous week to the training dataset. b. Model Retraining: Retrain the model on the expanded dataset. c. Performance Monitoring: Continuously track model performance on the newest data to ensure predictive power is maintained or improved [59].
Interpretation and Design:
- Explainable AI (XAI): For key predictions, use SHAP analysis to generate a beeswarm plot or dependence plots to show which molecular features (e.g., logP, presence of certain substructures) are driving the predicted stability value [60].
- Design-Make-Test-Analyze Loop: Chemists use the predictions and explanations to propose new compounds with improved predicted stability. These compounds are synthesized, tested, and the results are fed back into the model, closing the loop.
Workflow and Pathway Diagrams
Diagram Title: Integrated AI-PBPK ADME Optimization Workflow
Research Reagent Solutions
The following table lists key computational tools and resources essential for conducting AI-driven ADME prediction and PBPK modeling.
Table 2: Essential Research Reagents & Tools for AI-PBPK Modeling
| Item Name | Function / Application | Specifications / Notes |
|---|---|---|
| Curated Public ADME Dataset | Provides a benchmark dataset for training and validating ML models on endpoints like HLM/RLM stability, PPB, and solubility. | Includes 3,521 compounds with 316 RDKit molecular descriptors and 6 ADME endpoints. Essential for initial model development [60]. |
| Graph Neural Network (GNN) Architecture | The core ML model for learning structure-property relationships from molecular graphs. | Message-Passing Neural Networks (MPNN) are commonly used and have shown strong performance in predicting ADME properties for diverse molecules, including TPDs [61]. |
| SHAP (SHapley Additive exPlanations) | An Explainable AI (XAI) library for interpreting ML model predictions. | Quantifies the contribution of each molecular feature (descriptor) to a final prediction, moving models from "black box" to transparent [60]. |
| PBPK Software Platform | A simulation environment for building Physiologically Based Pharmacokinetic models. | Used to predict human PK, drug-drug interactions, and assess PK in special populations by integrating in vitro ADME data and system-specific physiology [62] [63] [66]. |
| RDKit | An open-source cheminformatics toolkit. | Used to calculate molecular descriptors and fingerprints from chemical structures, which serve as input features for many ML models [60]. |
Overcoming Bioavailability Challenges: Formulation Strategies and Ameliorating Toxicity
For researchers in drug development, addressing poor aqueous solubility is a critical hurdle, especially in toxicity testing where achieving adequate systemic exposure is paramount. A significant number of new chemical entities (NCEs) exhibit poor solubility, which can compromise bioavailability, lead to non-linear pharmacokinetics, and obscure toxicological assessment [67] [68]. This technical guide focuses on three primary solid-form strategies—salts, cocrystals, and amorphous solid dispersions (ASDs)—to overcome these challenges. The following FAQs and troubleshooting guides provide practical, experimental insights for scientists aiming to enhance solubility and ensure reliable results in preclinical studies.
FAQs: Core Concepts and Decision-Making
1. What is the fundamental difference between a salt, a cocrystal, and an amorphous solid dispersion in terms of molecular structure and properties?
- Salt: Forms when an ionic API (acid or base) reacts with a counterion (base or acid) via proton transfer. This creates an ionic bond, significantly altering the crystal lattice and properties like solubility, stability, and melting point. More than half of marketed small-molecule drugs are salts [69] [70].
- Cocrystal: Consists of an API and a co-former (a neutral molecule) in the same crystal lattice, connected by non-ionic interactions (e.g., hydrogen bonds). Cocrystals can modify physicochemical properties without changing the API's chemical structure and are applicable to non-ionizable molecules [67] [69].
- Amorphous Solid Dispersion (ASD): A single-phase, homogeneous mixture where the API is dispersed in a solid polymer matrix in an amorphous (non-crystalline) state. The high energy of the amorphous state can dramatically increase solubility and dissolution rate, but it is thermodynamically metastable and requires stabilization by polymers to prevent recrystallization [69] [71].
2. How do I decide which strategy is most appropriate for my poorly soluble compound?
The initial choice depends on your API's molecular characteristics. The following decision pathway can guide your initial strategy.
3. What are the key considerations for ensuring the physical stability of an Amorphous Solid Dispersion during storage?
Physical stability is the primary challenge for ASDs. The main risk is recrystallization, which negates the solubility advantage. Key strategies include:
- Polymer Selection: Use polymers that form strong intermolecular interactions (e.g., hydrogen bonds) with the API, which inhibit molecular mobility and crystallization. Common polymers include PVP, PVP-VA, and HPMC [69] [71].
- Drug Loading: Maintain the drug loading below the saturation solubility of the API in the polymer to prevent phase separation and crystallization [71].
- Storage Conditions: Store under controlled low humidity and temperature, as moisture can act as a plasticizer, increasing molecular mobility and promoting recrystallization [71].
4. Can these techniques be used in fixed-dose combination products?
Yes, and this is an area of growing interest. Drug-drug cocrystals/salts are crystalline materials containing two active pharmaceutical ingredients [69]. A prominent example is Entresto (sacubitril/valsartan), which is a co-crystal of two APIs. Similarly, ASDs can be designed to incorporate multiple drugs dispersed within a single polymer matrix, enabling synchronized release and improved compliance [69].
Troubleshooting Common Experimental Issues
Issue 1: Inconsistent or Failed Cocrystal Formation
Problem: Despite positive computational screening, cocrystals do not form experimentally.
| Possible Cause | Solution |
|---|---|
| Incorrect Stoichiometry | Systematically vary the molar ratios of API to co-former (e.g., 1:1, 2:1, 1:2) in your screening experiments. |
| Insufficient Activation Energy | The reaction mixture may not be receiving enough energy for molecular rearrangement. Increase grinding time in mechanochemical methods or consider using a small amount of solvent (solvent-drop grinding) to enhance molecular mobility [67]. |
| Unfavorable Solvent System | The solvent may be solubilizing one component preferentially. Screen a diverse set of solvents with different polarities and hydrogen-bonding capabilities for solvent-based methods [72]. |
| Thermodynamically Unstable Form | The cocrystal may be metastable. Use slurry ripening experiments in various solvents to convert to the most stable crystalline form [70]. |
Issue 2: Phase Separation or Recrystallization in Amorphous Solid Dispersions
Problem: The freshly prepared ASD shows crystals upon analysis, or crystals form during storage or dissolution.
| Possible Cause | Solution |
|---|---|
| Drug Loading Too High | The API concentration may exceed its solubility in the polymer matrix. Reduce the drug loading and re-formulate [71]. |
| Inadequate Polymer Selection | The polymer may not effectively inhibit API diffusion and crystallization. Screen alternative polymers (e.g., PVP-VA, HPMCAS) that have better miscibility and stronger interactions with your specific API [69] [71]. |
| Residual Crystallinity | The manufacturing process (e.g., spray drying, hot-melt extrusion) did not fully amorphize the API. Optimize process parameters like temperature, screw speed (HME), or solvent evaporation rate (spray drying) [67] [70]. |
| Poor Storage Conditions | Exposure to moisture or temperature fluctuations can plasticize the matrix. Store ASDs in desiccated containers at appropriate temperatures and consider using moisture-resistant packaging [71]. |
Issue 3: Dissolution Performance Does Not Translate to Bioavailability
Problem: The solid form shows excellent in vitro dissolution but fails to achieve expected exposure in in vivo toxicity studies.
| Possible Cause | Solution |
|---|---|
| Precipitation in GI Fluids | The drug forms a supersaturated solution but rapidly precipitates before absorption. Incorporate precipitation inhibitors (e.g., polymers like HPMC) into the formulation to maintain supersaturation [71]. |
| Poor Permeability | The drug belongs to BCS Class IV (low solubility, low permeability). Solubility enhancement alone is insufficient. Consider permeability enhancers or alternative delivery routes [68] [73]. |
| Drug-Rich Colloidal Phases | Upon dissolution, the drug may form amorphous or colloidal drug-rich particles. The bioavailability depends on the uptake from these complex systems, which may not be reflected in simple dissolution tests. Use advanced dissolution models (e.g., biphasic) to better simulate the in vivo environment [71]. |
Experimental Protocols for Key Screening Methodologies
Protocol 1: High-Throughput Cocrystal Screening via Solvent Drop Grinding
Objective: To rapidly screen multiple co-formers for their ability to form cocrystals with your API [67].
Materials:
- API
- Library of GRAS (Generally Recognized as Safe) co-formers
- Ball mill or vibrating mill
- HPLC vials or small grinding jars
- Organic solvents (e.g., methanol, acetonitrile, ethyl acetate)
Method:
- Prepare Mixtures: Weigh out 50-100 mg of a 1:1 molar ratio of API and co-former into a grinding jar.
- Add Solvent: Add 1-3 drops of a chosen solvent to the solid mixture. The solvent acts as a molecular lubricant but is not used in excess.
- Grind: Place the jar in the mill and grind for 30-60 minutes at a fixed frequency.
- Dry and Analyze: After grinding, transfer the solid material to a watch glass and allow any residual solvent to evaporate under a fume hood.
- Characterize: Analyze the resulting solid using Powder X-Ray Diffraction (PXRD) to identify new crystalline phases distinct from the starting materials. Confirm with techniques like Differential Scanning Calorimetry (DSC) and Fourier-Transform Infrared Spectroscopy (FTIR).
Protocol 2: Preparing an Amorphous Solid Dispersion via Hot-Melt Extrusion (HME)
Objective: To produce a homogeneous ASD of an API in a polymer matrix using HME technology [67] [70].
Materials:
- API
- Polymer (e.g., PVP-VA, HPMC)
- Hot-Melt Extruder (co-rotating twin-screw)
- Cryo-mill
- Desiccant
Method:
- Formulation Blend: Pre-blend the API and polymer at the desired ratio (e.g., 10-30% w/w drug loading) using a tumbler mixer for 15-30 minutes.
- Extruder Setup: Set the temperature profile of the extruder barrels to above the glass transition temperature (Tg) of the polymer but below the melting point of the crystalline API to prevent degradation. The screw configuration should include conveying and mixing elements.
- Feeding and Extrusion: Feed the physical mixture into the extruder hopper at a constant rate. Monitor torque to ensure homogeneity.
- Collection: Collect the extrudate as it exits the die. Allow it to cool on a cooling belt or tray.
- Size Reduction: Mill the cooled, brittle extrudate into a fine powder using a cryo-mill to prevent heat-induced crystallization.
- Characterization and Storage: Analyze the powder by PXRD to confirm the absence of crystallinity. Store the final ASD in a desiccated container at controlled room temperature.
The Scientist's Toolkit: Essential Research Reagents
| Reagent / Material | Function in Solubility Enhancement |
|---|---|
| Polyvinylpyrrolidone-vinyl acetate (PVP-VA) | A common polymer used in ASDs to inhibit crystallization and maintain supersaturation via hydrogen bonding [71]. |
| Methanesulfonic Acid | A pharmaceutically acceptable counterion for forming salts with basic APIs, often leading to high solubility [70]. |
| Nicotinamide | A widely used GRAS co-former in cocrystal screening that can form heterosynthons with carboxylic acids and other hydrogen bond donors [67]. |
| Diatomaceous Earth | The solid support in Supported Liquid Extraction (SLE), used to isolate analytes from complex biological matrices during bioanalysis, helping to avoid emulsions common in LLE [74]. |
| Hydroxypropyl Methylcellulose Acetate Succinate (HPMCAS) | A polymer for ASDs that provides pH-dependent release and acts as an effective precipitation inhibitor in the intestine [71]. |
Technique Selection and Problem Resolution Workflow
The following diagram illustrates a logical workflow for navigating solubility challenges, from initial analysis to problem resolution, integrating the concepts from this guide.
Within the context of toxicity testing and environmental risk assessment, bioavailability refers to the fraction of a contaminant that can be readily taken up by an organism, exerting a physiological or toxicological effect. For soil-dwelling organisms and plants, this is not the total concentration of a contaminant, but rather its environmentally available fraction that dissolves into pore water or is otherwise accessible for uptake [75]. In situ immobilization using soil amendments is a cornerstone strategy for managing contaminated environments. This approach centers on adding substances to soil that alter its physicochemical properties, thereby reducing the bioavailability of contaminants without removing them from the matrix. This technical guide focuses on two prominent amendments—biochar and calcium carbonate—detailing their mechanisms, applications, and troubleshooting for researchers in drug development and environmental toxicology.
Core Mechanisms of Contaminant Immobilization
How Biochar Immobilizes Contaminants
Biochar, a carbon-rich material produced from the pyrolysis of biomass, immobilizes contaminants through several simultaneous mechanisms [76] [77] [78]:
- Surface Complexation: The diverse oxygen-containing functional groups (e.g., carboxyl, hydroxyl) on biochar's surface act as ligands, forming strong complexes with cationic heavy metals like Cadmium (Cd), Lead (Pb), and Copper (Cu). Acid modification of biochar can significantly increase the density of these functional groups, enhancing its complexation capacity [78].
- Precipitation: Biochar's generally alkaline nature can increase soil pH, promoting the precipitation of metal ions as less soluble hydroxides, carbonates, or phosphates [77]. For instance, the ash content in manure-derived biochar can provide ions that facilitate the co-precipitation of metals [78].
- Cation Exchange: The inherent cation exchange capacity (CEC) of biochar allows it to retain positively charged metal ions on its surface, exchanging them for more innocuous cations like Ca²⺠or K⺠[78].
- Physical Adsorption: Its high specific surface area and porous structure enable the physical entrapment of both organic and inorganic contaminants [78].
The following diagram illustrates the primary immobilization pathways for biochar:
How Calcium Carbonate Immobilizes Contaminants
Calcium carbonate (CaCO₃), particularly in its metastable vaterite form, operates through distinct pathways [79] [80]:
- Co-precipitation: During the microbially induced carbonate precipitation (MICP) process, heavy metal ions with a similar ionic radius to Ca²⺠(e.g., Pb²âº, Sr²âº) can be incorporated directly into the growing crystal lattice of calcium carbonate, effectively trapping them within a mineral matrix [80].
- Surface Sorption: The high specific surface area of porous vaterite allows for the adsorption of contaminants onto its surface [79].
- Alkaline Hydrolysis: The dissolution of calcium carbonate can increase the pH of the local microenvironment, promoting the hydrolysis and precipitation of metal cations [80].
The following diagram illustrates the primary immobilization pathways for calcium carbonate:
Troubleshooting Guide: FAQs and Solutions
Q1: My amendment successfully immobilized cadmium (Cd), but it increased the bioavailability of arsenic (As). What went wrong?
- Problem: This is a classic issue of divergent pH dependence. Cadmium bioavailability typically decreases as soil pH rises due to precipitation and stronger sorption. In contrast, arsenic, an oxyanion (e.g., AsO₄³â»), often becomes more mobile and bioavailable under alkaline conditions because the sorption sites on soil minerals become negatively charged, leading to electrostatic repulsion [81].
- Solution: Use a combined or modified amendment that can target both cationic and anionic contaminants simultaneously.
- Iron-Modified Biochar: Loading iron oxides onto biochar creates a material that can adsorb arsenate anions through specific ligand exchange while also immobilizing cadmium via the mechanisms described above [81].
- Lime + Ferrous Sulfate (LF) Combination: The lime component immobilizes Cd, while the ferrous sulfate provides a source of Fe ions that can form Fe-(hydr)oxides, which are potent adsorbents for As [81].
Q2: The immobilization effect in my sandy loam soil is significantly less effective than in a silty clay loam. Why?
- Problem: The efficacy of amendments is highly dependent on soil texture. Light-textured, sandy soils generally have:
- Lower native cation exchange capacity (CEC).
- Less surface area for amendment-contaminant interactions.
- Higher permeability, which can lead to faster leaching of both contaminants and dissolved amendment components [78].
- Solution:
- Increase the application rate of the amendment for sandy soils to compensate for the lower inherent retention capacity.
- Select an amendment with high surface activity. Acid-modified biochars, for instance, create abundant oxygen functional groups that enhance complexation with metals, which can be particularly beneficial in soils with low clay content [78].
Q3: I am using calcium carbonate, but I'm concerned about its long-term stability. How can I ensure a lasting effect?
- Problem: Pure, synthetic vaterite is thermodynamically unstable and can transform in aqueous environments over 20-25 hours into the more stable calcite, potentially re-releasing trapped contaminants [79].
- Solution:
- Utilize biogenic vaterite. Research shows that vaterite induced by bacteria like Bacillus subtilis incorporates organic molecules (proteins) from the microbial process. These organics act as stabilizers, preventing phase transformation and maintaining the mineral's structure and contaminant-holding capacity for over a year [79].
- Explore polymer-stabilized or composite materials that can mimic this stabilizing effect.
Q4: How can I directly and reliably measure the success of an immobilization treatment in terms of reduced bioavailability?
- Problem: Chemical extraction of total contaminants does not reflect the bioavailable fraction.
- Solution: Employ a combination of chemical and biological assays.
- Chemical Assessment: Perform a sequential extraction procedure (e.g., BCR method). A successful treatment will show a shift in the contaminant from the "soluble and exchangeable" fraction (bioavailable) to more stable fractions like "organic matter-bound" or "residual" [78].
- Biological Assessment (Bioassay): Use standard organisms like earthworms (Eisenia veneta). Measure the bioaccumulation factor (BSAF) in the organisms exposed to treated vs. untreated soil. A significant reduction in BSAF is a direct measure of reduced bioavailability and toxicity [75].
Research Reagent Solutions: Essential Materials
Table 1: Key Research Materials for Immobilization Studies
| Reagent/Material | Key Function & Properties | Research Application Notes |
|---|---|---|
| Sheep Manure Biochar | High ash content, rich in nutrients and functional groups. | Particularly effective when acid-modified (HNO₃) for Cd immobilization in calcareous soils [78]. |
| Iron-Modified Biochar (MB) | Biochar loaded with iron oxides; targets both cations (Cd) and anions (As). | Ideal for co-contaminated soils. Preparation involves impregnating biochar with Fe salts (e.g., FeCl₃) [81]. |
| Vaterite (CaCO₃) | Metastable polymorph of calcium carbonate; high porosity and specific surface area. | Biogenic vaterite induced by Bacillus subtilis offers superior stability over synthetic versions [79]. |
| Ureolytic Bacteria (e.g., Pseuduginosa, P. rettgeri) | Hydrolyze urea to produce carbonate ions (CO₃²â»), inducing CaCO₃ precipitation. | Used in Microbially Induced Carbonate Precipitation (MICP). Selected strains can tolerate heavy metals and co-precipitate them with high efficiency [80]. |
| Earthworms (Eisenia veneta) | Standard bioindicator organisms for soil toxicity. | Used in bioassays to measure the bioaccumulation factor (BSAF), providing a direct assessment of toxicological bioavailability [75]. |
Detailed Experimental Protocols
Protocol: Acid Modification of Biochar for Enhanced Metal Sorption
This protocol is adapted from methods used to significantly increase the density of oxygen functional groups on biochar, boosting its complexation capacity for metals like Cd [78].
- Materials: Unmodified biochar (e.g., from sheep manure or rice husk), 25% Nitric Acid (HNO₃) solution, Deionized water, Heating mantle with reflux condenser, Filtration setup (Buchner funnel and filter paper), Oven.
- Procedure:
- Weigh 10 g of dry, unmodified biochar.
- In a fume hood, add the biochar to 300 mL of a 25% HNO₃ solution in a round-bottom flask.
- Attach a reflux condenser and heat the mixture to 90°C for 4 hours with continuous stirring.
- After cooling, filter the mixture using a Buchner funnel and collect the solid.
- Thoroughly wash the acid-modified biochar with deionized water until the filtrate reaches a neutral pH.
- Dry the washed biochar in an oven at 105°C for 24 hours.
- Grind and sieve the final product to a uniform particle size (e.g., <0.5 mm) before application.
- Troubleshooting Tip: Incomplete washing will leave residual acid, which can drastically lower the pH of the test soil and potentially increase metal mobility. Always verify the final pH of the wash water is neutral.
Protocol: Microbially Induced Carbonate Precipitation (MICP) for Metal Immobilization
This protocol outlines the process of using ureolytic bacteria to precipitate calcium carbonate and co-precipitate heavy metals, achieving high removal efficiencies [80].
- Materials:
- Bacterial Strains: Select a robust, ureolytic, and metal-tolerant strain (e.g., Pseudomonas aeruginosa QZ9 or Providencia rettgeri QZ2 from collections).
- Culture Media:
- LB Broth: For initial growth.
- Urea Medium (UM): Contains (per liter): NaCl 5.0 g, Peptone 0.2 g, Glucose 1.0 g, KHâ‚‚POâ‚„ 2.0 g, and filter-sterilized Urea 20 g.
- Metal Solution: A sterile aqueous solution of the target metal salt (e.g., CdClâ‚‚).
- Calcium Source: Sterile CaClâ‚‚ solution.
- Procedure:
- Culture Preparation: Inoculate the bacterial strain in LB broth and incubate until mid-log phase. Harvest cells by gentle centrifugation and wash with sterile saline to remove residual media.
- MICP Reaction: Resuspend the bacterial cells in UM to an OD₆₀₀ of approximately 0.15. Add the target heavy metal and CaCl₂ (e.g., 0.5 M final concentration).
- Incubation: Incubate the culture at 30°C with shaking (200 rpm) for 3-5 days.
- Analysis: After incubation, centrifuge the culture. Analyze the supernatant for residual metal concentration (e.g., via AAS/ICP) to determine removal efficiency. Analyze the precipitate mineralogy using X-ray diffraction (XRD) and morphology using scanning electron microscopy (SEM).
- Troubleshooting Tip: Low precipitation efficiency can result from bacterial toxicity. Always determine the minimum inhibitory concentration (MIC) of the target heavy metal for your specific bacterial strain prior to the main experiment [80].
Fundamental Concepts & FAQs
FAQ 1: What is the core advantage of combining nanocarriers with 3D printing for drug delivery? The synergy lies in overcoming the limitations of each technology when used alone. Nanocarriers improve drug solubility, stability, and cellular uptake but are challenging to formulate into solid dosage forms. 3D printing enables the fabrication of sophisticated, patient-specific solid dosage forms (like tablets or implants) that can precisely encapsulate and control the release of these nanocarriers, thereby enhancing bioavailability and enabling personalized dosing [82] [83].
FAQ 2: Why is bioavailability a critical parameter in toxicity testing and drug development? Bioavailability determines the proportion of a drug that reaches systemic circulation and its target site. In toxicity testing, low or variable bioavailability can lead to inaccurate results—either masking a drug's true toxic effects or failing to demonstrate its therapeutic efficacy. Advanced delivery systems aim to provide consistent and sufficient bioavailability to ensure toxicity studies are reliable and predictive of clinical outcomes [84].
FAQ 3: What are the primary types of 3D printing used with nanocarrier-loaded formulations? The two most prominent techniques are Fused Deposition Modeling (FDM), which uses thermoplastic filaments, and Pressure-Assisted Microsyringe (PAM) or Semi-Solid Extrusion (SSE), which extrudes pastes or gels. Both are extrusion-based methods suitable for incorporating sensitive nanocarriers like polymeric nanocapsules or Self-Nanoemulsifying Drug Delivery Systems (SNEDDS) into solid dosage forms without destroying their nanostructure [82].
FAQ 4: What safety considerations are specific to 3D printing medical or drug delivery devices? For devices printed from photopolymer resins, incomplete post-processing (washing and curing) can leave cytotoxic, unreacted monomers on the final product. Biocompatibility is a property of the correctly processed final part, not the raw resin. A rigorously validated post-processing workflow is essential to prevent the transfer of toxic leachables to patients and to ensure dimensional accuracy [85].
Troubleshooting Common Experimental Issues
Nanocarrier Formulation and Characterization
Table 1: Troubleshooting Nanocarrier Performance
| Problem | Potential Cause | Solution |
|---|---|---|
| Low Drug Encapsulation Efficiency | Rapid drug diffusion during formulation; inappropriate core/shell material ratio. | Optimize the microfluidic flow rate ratio (FRR) to control mixing time and self-assembly. Use a pre-formulation solubility screen to select core materials with higher affinity for the drug [86]. |
| High Polydispersity Index (PDI) | Aggregation of particles; inconsistent nucleation and growth during synthesis. | Use microfluidic synthesis for superior control over mixing, resulting in a narrower size distribution compared to bulk methods. Implement purification steps like asymmetrical flow field-flow fractionation (AF4) to isolate monodisperse fractions [87] [86]. |
| Poor Cellular Uptake | Non-optimal surface charge (zeta potential) or hydrophobicity. | Fine-tune the surface chemistry. A moderately positive zeta potential may enhance interaction with negatively charged cell membranes. Use techniques like X-ray photon correlation spectroscopy to characterize surface groups and adjust coating materials accordingly [87]. |
| Nanocarrier Instability in Storage | Ostwald ripening; chemical degradation; surface property changes. | Lyophilize (freeze-dry) with appropriate cryoprotectants for long-term storage as a solid. For liquid suspensions, ensure storage at 4°C and protect from light [87]. |
3D Printing of Nanocarrier-Loaded Formulations
Table 2: Troubleshooting 3D Printing Processes
| Problem | Potential Cause | Solution |
|---|---|---|
| Nozzle Clogging During Printing | Nanocarrier aggregation in the printing ink/filament; particle size too large for nozzle diameter. | Ensure nanocarriers are monodisperse and filter the ink precursor. For FDM, optimize the filament diameter and printer nozzle temperature to ensure smooth flow [82] [83]. |
| Inconsistent Drug Release Profile | Inadequate washing or curing of the 3D printed structure; suboptimal internal geometry. | Validate the post-processing workflow. Ensure complete resin removal and full UV curing to create a stable polymer network. Design and print tablets with complex internal geometries (e.g., lattices) to better control surface area and release kinetics [83] [85]. |
| Low Mechanical Strength of Printed Dosage Form | Under-curing of photopolymers; incorrect polymer blend for FDM; high porosity. | For resins, validate the curing time and intensity, potentially using an oxygen-free (e.g., glycerine) environment for better polymerization. For FDM, use polymer blends (e.g., PLA-PEG) to improve flexibility and strength [85]. |
| Loss of Nanocarrier Integrity Post-Printing | Excessive shear force during extrusion; high printing temperature degrading the API. | For shear-sensitive carriers, use the PAM/SSE technique over FDM. For FDM, select a polymer matrix with a lower melting point and incorporate thermostable nanocarriers [82]. |
Detailed Experimental Protocols
Protocol 1: Formulating Solid Dosage Forms from Liquid SNEDDS using PAM 3D Printing
This protocol transforms a liquid self-nanoemulsifying drug delivery system (SNEDDS) into a solid, customizable tablet, enhancing dose flexibility and stability [82].
1. Research Reagent Solutions Table 3: Essential Materials for PAM 3D Printing of SNEDDS
| Item | Function |
|---|---|
| Liquid SNEDDS Pre-concentrate | Contains drug, oil, surfactant, and co-surfactant; forms nanodroplets upon aqueous dilution. |
| Solid Carrier (e.g., Aerosil 200) | Porous silica adsorbent that absorbs the liquid SNEDDS to form a solid, printable paste. |
| Bioink Binder (e.g., PEG 400) | Plasticizer that provides suitable rheology for extrusion and binding of the final tablet. |
| Pressure-Assisted Microsyringe (PAM) | 3D printer that uses pneumatic pressure to extrude semi-solid materials at room temperature. |
2. Methodology
- Step 1: Paste Preparation. The liquid SNEDDS is gradually added to the solid carrier (Aerosil 200) in a weight ratio of approximately 1:1 to 3:1 (SNEDDS:carrier) and mixed thoroughly in a mortar until a homogeneous, damp powder is achieved. A small amount of PEG 400 (e.g., 2-5% w/w) is then added and mixed to form a cohesive, extrudable paste.
- Step 2: Printer Setup. Load the paste into a syringe barrel. Attach the syringe to the PAM printer and select an appropriate nozzle diameter (e.g., 0.4-0.8 mm). Set the printing parameters: pneumatic pressure (20-80 kPa), printing speed (5-15 mm/s), and layer height (50-80% of nozzle diameter).
- Step 3: Printing & Curing. Design a tablet model (e.g., 10mm diameter, 3mm height) using CAD software and generate the G-code. Print the tablet layer-by-layer. After printing, the tablets may be air-dried or placed in a desiccator for 24 hours to remove residual moisture and solidify.
3. Validation and Characterization
- Drug Release: Use USP dissolution apparatus II (paddle method) in a pH 6.8 phosphate buffer. Analyze drug concentration in the medium over time using HPLC to confirm the SNEDDS's rapid release profile is maintained.
- Tablet Morphology: Use Scanning Electron Microscopy (SEM) to examine the surface and internal structure for homogeneity and absence of cracks.
- Content Uniformity: Test 10 individual tablets according to pharmacopeial standards to ensure consistent drug dosage.
Diagram 1: PAM 3D Printing of SNEDDS Tablets
Protocol 2: Assessing Cytotoxicity of 3D Printed Medical Devices
This protocol is critical for ensuring the safety of 3D printed devices, especially those made from photopolymer resins, by detecting any residual cytotoxic leachables [85].
1. Research Reagent Solutions Table 4: Essential Materials for Cytotoxicity Testing
| Item | Function |
|---|---|
| Test Device Sample | The final, post-processed 3D printed device or a representative sample. |
| Cell Culture (e.g., L929 mouse fibroblast cells) | Standardized cell line used for biocompatibility testing according to ISO 10993-5. |
| Culture Medium (e.g., DMEM with serum) | Nutrient medium for cell growth and as the extraction vehicle. |
| Incubator (37°C, 5% CO₂) | Maintains optimal physiological conditions for cell growth. |
2. Methodology (ISO 10993-5 Elution Method)
- Step 1: Extract Preparation. Sterilize the test device sample. Place the sample in a culture medium at a surface area-to-volume ratio of 3-6 cm²/mL. Incubate the mixture at 37°C for 24 hours to create the "extract." Prepare a fresh culture medium as a negative control.
- Step 2: Cell Seeding and Exposure. Seed L929 cells in a multi-well plate and incubate until a near-confluent monolayer is formed. Remove the growth medium and replace it with the device extract (test group) and fresh medium (negative control). Incubate the plates for 24-72 hours.
- Step 3: Microscopic Evaluation. After incubation, examine the cell monolayers under a microscope. Assess the degree of cell lysis (death), membrane damage, and overall morphological changes compared to the negative control.
3. Interpretation of Results
- Grade 0 (None): No cell lysis or reactivity. The device is non-cytotoxic.
- Grade 1 (Slight): Less than 20% of cells are affected.
- Grade 2 (Mild): 20% to 40% of cells are affected. (Considered the upper limit of acceptance, indicates low safety margin).
- Grade 3 (Moderate): 40% to 60% of cells are affected. (Indicates a failed, cytotoxic device).
- Grade 4 (Severe): 60% to 100% of cells are lysed. (Indicates a severely cytotoxic device) [85].
Diagram 2: Cytotoxicity Testing Workflow
Advanced Support: Addressing 3D Printing Emissions
Issue: Fused Filament Fabrication (FFF) 3D printing can release ultrafine particles (UFPs) and volatile organic compounds (VOCs) like styrene, which pose an inhalation risk in the lab and could confregate toxicity studies [88].
Risk Mitigation Strategies:
- Ventilation: Always operate 3D printers in a well-ventilated area, ideally within a fume hood or a separately ventilated room.
- Temperature Control: Use the lowest possible printing temperature that still ensures good print quality, as higher temperatures correlate with higher emissions.
- Material Selection: Be cautious with filaments containing particulate additives (e.g., carbon nanotubes) and choose low-emission filaments where possible [88].
- Exposure Monitoring: Use real-time air particle monitors in labs with frequent 3D printing activity to assess UFP levels.
Frequently Asked Questions (FAQs)
In the context of bioavailability and toxicity testing, observed variation in response can be broken down into several independent components [89]:
- Between-Biological Subjects (B): The natural variation between individuals (e.g., patients, animals) given the same treatment.
- Biological Subject-by-Treatment Interaction (C): The extent to the effects of treatments vary from subject to subject; this is the core of personalized medicine.
- Within-Subject (D): The variation from occasion to occasion when the same subject is given the same treatment.
To formally assess the precision of your high-throughput assay, the recommended statistical quantity is repeatability (R), also known as the intraclass correlation coefficient (ICC) [90]. It is defined for an analyte k as:
R(k) = Biological Signal Variance / (Biological Signal Variance + Experimental Noise Variance)
This metric, which ranges from 0 to 1, tells you the proportion of total variance attributable to true biological signal versus experimental noise. A value close to 1 indicates high precision [90].
Why is a high correlation between technical replicates sometimes misleading for assay precision?
A common but flawed practice is to scatterplot two technical replicates and report a high sample correlation coefficient (r≈1) as proof of assay precision. This can be misleading because the correlation is confounded by the assay's dynamic range [90].
A high correlation can occur even when experimental noise is large, provided the dynamic range of measurements across different analytes is even larger. Therefore, a high r does not guarantee that your noise is small relative to the biological signal you are trying to detect. The repeatability (R), which separates the biological signal from experimental noise, is a more reliable and informative metric [90].
How can I improve the reliability and interpretability of my statistical models for complex data?
Integrating knowledge of your study design directly into the statistical analysis can significantly improve model quality. One powerful approach is combining Analysis of Variance (ANOVA) with multivariate regression methods like Partial Least Squares (PLS) [91].
The ANOVA-PLS method works by [91]:
- Using ANOVA to first decompose the total dataset into independent data blocks associated with specific design factors (e.g., time, diet, batch).
- Then, applying PLS regression to the relevant combination of these data blocks to model the relationship between your omics data (e.g., lipidomics) and a phenotype (e.g., an inflammation marker).
This process strips away structured noise and irrelevant sources of variation, leading to more reliable, better-interpretable models and the identification of more biologically relevant metabolites [91].
Troubleshooting Guides
Problem: Inability to Distinguish True Biological Signal from Experimental Noise
Issue: Your results are inconsistent, and you suspect that experimental variability is obscuring true biological effects, a critical problem when assessing the bioavailability and toxicity of complex molecules.
Solution:
- Conduct a Pilot Repeatability Study: Incorporate technical replicates into a pilot study design. This involves splitting biological samples into aliquots and analyzing them separately [90].
- Estimate Variance Components: Use statistical methods like Analysis of Variance (ANOVA) to estimate the biological signal variance and experimental noise variance for your key analytes [90].
- Calculate Repeatability: Compute the repeatability (R) for each analyte. This will help you identify which measurements are sufficiently precise for your study goals [90].
- Inform Full Study Design: Use the estimated repeatability to perform a formal sample size calculation. This ensures your main experiment has sufficient statistical power to detect effects of biological interest.
Problem: Statistical Model is Unreliable or Difficult to Interpret
Issue: A standard multivariate regression model (e.g., PLS) applied to your entire dataset performs poorly or yields results that are biologically uninterpretable.
Solution:
- Decompose the Data: Apply an ANOVA model that reflects your experimental design (e.g.,
Response = Overall Mean + Time + Diet + (Time*Diet) + Residual). This separates the data into orthogonal blocks for each factor [91]. - Apply Regression to Relevant Subsets: Instead of modeling the raw data, build your PLS model using only the data blocks that contain the variation of interest. For example, to find metabolites related to a diet-induced inflammatory response, you might use the 'Diet' and 'Time x Diet' interaction effect blocks [91].
- Validate the Model: Use standard cross-validation techniques on the ANOVA-PLS model and compare its performance and interpretability to the standard PLS model. This approach often leads to the discovery of more relevant biomarkers [91].
Key Data and Experimental Protocols
Variance Components in Different Study Designs
The type of clinical trial or experiment you run determines which components of variation you can actually identify and estimate [89].
| Type of Trial | Description | Identifiable Components of Variation |
|---|---|---|
| Parallel Group | Patients are randomized to a single course of one treatment. | Treatment Effect (A) |
| Classical Cross-Over | Patients are randomized to sequences of treatments, one per period. | A, Between-Patient (B) |
| Repeated Period Cross-Over | Patients are randomized to sequences where each treatment is given in more than one period. | A, B, Patient-by-Treatment Interaction (C) |
Source: Adapted from Senn (2015) [89].
Protocol for Assessing Assay Repeatability
Objective: To quantify the repeatability (R) of a high-throughput assay for use in sample size planning.
Methodology [90]:
- Pilot Study Design: Select a set of biological samples (e.g., from 10-15 subjects). For each sample, prepare and run at least 2 technical replicates.
- Data Collection: Run all samples and replicates through the assay, measuring all
panalytes. - Variance Estimation: For each analyte
k, use ANOVA or restricted maximum likelihood (REML) methods to estimate:v_b(k): The variance of the biological signal.v_e(k): The variance of the experimental noise.
- Calculate Repeatability: For each analyte, compute
R(k) = v_b(k) / (v_b(k) + v_e(k)). - Application: Use the distribution of
R(k)values across analytes to determine how many biological replicates are needed in future studies to achieve sufficient power.
Experimental Workflow and Signaling Pathways
Statistical Modeling Workflow with ANOVA-PLS
This diagram illustrates the process of decomposing complex data using study design information to build a more reliable statistical model.
Variance Components in Experimental Data
This diagram breaks down the total variation in a measurement into its key statistical components.
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in Experiment |
|---|---|
| Technical Replicates | Aliquots from the same biological sample used to run the assay multiple times; essential for estimating experimental noise variance and calculating repeatability [90]. |
| ANOVA-Based Software | Statistical software (e.g., R, Python with appropriate libraries) capable of performing variance component analysis to decompose data according to the experimental design [91] [90]. |
| PLS Regression Tools | Multivariate statistical software for performing Partial Least Squares regression, which is used to model relationships between different data blocks (e.g., omics data and clinical phenotypes) [91]. |
| High-Throughput Assay | The platform (e.g., LC-MS, RNA-Seq) used to simultaneously measure multiple analytes from a single sample, generating the complex data that requires careful variance analysis [90]. |
Frequently Asked Questions
1. What are the most common factors that reduce oral bioavailability in preclinical models? The most common factors can be categorized into three areas, each with distinct mechanisms:
- Dietary Factors: The presence of specific foods can significantly alter metabolic enzyme activity. For example, cruciferous vegetables may induce CYP1A enzymes, increasing first-pass metabolism, while grapefruit juice inhibits CYP3A, potentially increasing bioavailability for its substrates [92].
- Age-Related Changes: Aging is associated with reduced liver volume and blood flow, which can decrease first-pass metabolism for some drugs, leading to higher bioavailability. Conversely, age-related reduction in absorptive surface area or active transport mechanisms (e.g., for Vitamin B12, iron, calcium) can decrease absorption [93] [12].
- Disease States: Liver diseases, such as cirrhosis, can severely impair metabolic enzyme activity and cause vascular shunting, allowing drug-containing blood to bypass the liver. This can lead to a dramatic increase in the bioavailability of drugs that normally undergo extensive first-pass metabolism [92].
2. How can I quickly diagnose the primary cause of low bioavailability for a new chemical entity? Initial diagnosis should focus on profiling the compound's fundamental properties and then designing targeted in vivo studies. The table below outlines a strategic approach [94]:
Table: Diagnostic Strategy for Low Bioavailability
| Investigation Step | Method/Test | Interpretation of Results |
|---|---|---|
| Property Profiling | In vitro solubility and permeability assays (e.g., Caco-2, PAMPA) [94]. | Low solubility and/or low permeability suggests an absorption-limited problem (FAbs). |
| First-Pass Effect | Compare bioavailability after oral and intraportal venous administration in rodents [94]. | A significant increase in bioavailability with intraportal dosing indicates significant hepatic first-pass metabolism (FH). |
| Gut vs. Liver Metabolism | Compare bioavailability after oral and intraduodenal dosing with intravenous dosing [92]. | Allows differentiation between gastrointestinal (FG) and hepatic (FH) first-pass extraction. |
3. What formulation strategies can mitigate low bioavailability caused by poor solubility? For compounds with poor aqueous solubility, which is a common challenge in drug discovery, several formulation strategies can be employed in preclinical studies [94]:
- Solution Dosing Vehicles: Use pharmaceutically accepted solvents (e.g., PEG 400) and surfactants (e.g., polysorbate 80) to create a solution formulation, which provides the best chance for absorption by removing dissolution as a barrier.
- Lipid-Based Formulations: These can enhance the solubility and absorption of lipophilic compounds by facilitating formation of mixed micelles and promoting lymphatic transport [95] [94].
- Amorphous Solid Dispersions: Dispersing the drug in an amorphous polymer matrix can significantly increase the apparent solubility and dissolution rate compared to the crystalline form [96].
- Particle Size Reduction (Nanonization): Reducing particle size increases the surface area, which can dramatically enhance the dissolution rate [96].
4. Are there specific dietary controls needed for animal studies to ensure reproducible bioavailability data? Yes, diet is a critical variable. To minimize inter-study variability:
- Standardize Diet: Use a consistent, standardized laboratory diet throughout a study series.
- Control Feeding: Implement controlled fasting and feeding schedules, as food can alter gastrointestinal pH, motility, and bile flow.
- Avoid Inducers/Inhibitors: Be aware that certain laboratory chows may contain constituents (e.g., phytoestrogens, indoles) that can modulate enzyme activity. The use of purified diets may be necessary for highly sensitive assays [92].
Troubleshooting Guides
Guide 1: Addressing Diet-Induced Variability
Dietary components are a major source of variability in presystemic metabolism.
Table: Common Dietary Factors Affecting Bioavailability
| Dietary Factor | Effect on Metabolism | Impact on Bioavailability | Suggested Action |
|---|---|---|---|
| Grapefruit Juice | Inhibits intestinal CYP3A [92]. | Marked increase for CYP3A substrates. | Strictly avoid in study subjects (human/animal); use controlled water. |
| Cruciferous Vegetables (e.g., Brussels sprouts) | Induces CYP1A via Ah-receptor [92]. | Decrease for CYP1A substrates. | Exclude from diet for a defined period (e.g., 1-2 weeks) prior to and during studies. |
| Charcoal-Broiled/Smoked Foods | Induces xenobiotic metabolizing enzymes (e.g., CYP1A) [92]. | Decrease for substrates of induced enzymes. | Use standardized, non-grilled diets in animal models. |
| High-Fat Meal | Increases bile secretion and lymphatic flow [95]. | Can increase absorption of lipophilic compounds. | Standardize fasting conditions or administer with a controlled meal. |
| Fiber & Phytates (in plant-based foods) | Can bind to drugs and minerals, reducing absorption [95]. | Decreased absorption. | Account for matrix effects; consider purified diets for mineral studies. |
Guide 2: Accounting for Age-Related Physiological Changes
Aging results in physiological changes that can significantly alter pharmacokinetics. The following diagram summarizes the key age-related changes impacting the absorption and metabolism of compounds.
The table below details these changes and their experimental implications.
Table: Age-Related Changes and Experimental Considerations
| Physiological Change | Impact on Bioavailability & PK | Troubleshooting Strategy |
|---|---|---|
| Reduced Liver Volume & Blood Flow [93] | Reduced first-pass metabolic capacity, leading to increased bioavailability of high-extraction-ratio drugs [93]. | Use age-appropriate animal models; anticipate higher systemic exposure and adjust doses for elderly populations. |
| Reduced Active Transport [93] | Decreased absorption of nutrients and drugs that rely on active processes (e.g., Vitamin B12, iron, calcium, levodopa) [93]. | For compounds dependent on transporters, validate absorption models in aged specimens. |
| Altered Body Composition (↑ body fat, ↓ lean mass) [93] | Increased volume of distribution (V) for lipid-soluble drugs, prolonging elimination half-life [93]. | Monitor drug accumulation; loading doses may need adjustment based on V. |
| Reduced Gastric Acid Secretion [93] | Can alter the solubility and dissolution of ionizable drugs, potentially increasing or decreasing their absorption [93]. | Control for gastric pH in experimental design; its impact is drug-specific. |
Guide 3: Mitigating the Impact of Disease States
Disease states, particularly those affecting the liver and kidneys, can profoundly alter drug disposition.
Liver Disease (e.g., Cirrhosis):
- Mechanism: Impaired metabolic enzyme activity and the development of intra- and extra-hepatic vascular shunts, which bypass functional liver tissue [92].
- Impact: Can lead to a several-fold increase in the oral bioavailability of drugs that are normally extensively metabolized on the first pass (e.g., those with >80% first-pass effect in healthy subjects) [92].
- Protocol: In animal models, induce specific disease states (e.g., using carbon tetrachloride for liver fibrosis) and compare PK parameters to healthy controls. In clinical studies, stratify patients by disease severity using standardized scoring systems (e.g., Child-Pugh score).
Gastrointestinal Diseases:
- Mechanism: Conditions like inflammatory bowel disease (IBD) can alter gut motility, permeability, and the expression and activity of metabolic enzymes and transporters in the intestinal epithelium.
- Impact: Highly variable and disease-specific, potentially leading to either increased or decreased and more erratic absorption.
- Protocol: Utilize gut-specific sampling techniques (e.g., loco-regional absorption measurements) in relevant animal models to dissect the complex changes.
The Scientist's Toolkit: Key Experimental Protocols
Protocol 1: In Vitro Permeability Assessment using Caco-2 Cells
This protocol is a standard for predicting intestinal absorption potential during early drug discovery [94].
Objective: To determine the apparent permeability (Papp) of a test compound across a monolayer of Caco-2 cells, a model of the human intestinal epithelium.
Materials:
- Caco-2 cell line
- Transwell cell culture inserts (e.g., 12-well, 1.12 cm² surface area, 0.4 µm pore size)
- Transport buffer (e.g., HBSS, with or without pH adjustment)
- Test compound
- LC-MS/MS system for analytical quantification
Method:
- Cell Culture: Seed Caco-2 cells onto Transwell inserts and culture for 21-28 days to allow for full differentiation and formation of tight junctions. Monitor integrity by measuring transepithelial electrical resistance (TEER).
- Experiment Setup: Pre-wash the cell monolayers with transport buffer. Add the test compound (typically 10-100 µM) to the donor compartment (apical for A→B transport, basolateral for B→A transport).
- Incubation: Place the plates on an orbital shaker in an incubator (37°C). At predetermined time points (e.g., 30, 60, 90, 120 min), sample aliquots from the receiver compartment.
- Sample Analysis: Quantify the concentration of the test compound in the receiver and donor samples using a validated LC-MS/MS method.
- Data Calculation: Calculate the Papp (in cm/s) using the formula: Papp = (dQ/dt) / (A × C₀) Where dQ/dt is the flux rate (mol/s), A is the membrane surface area (cm²), and C₀ is the initial donor concentration (mol/mL).
Protocol 2: Assessing the Food Effect
This in vivo protocol is critical for understanding how diet influences bioavailability.
Objective: To evaluate the effect of food on the rate and extent of absorption of an orally administered test compound.
Materials:
- Laboratory animals (e.g., rats, beagles)
- Standard laboratory diet or a specific high-fat diet
- Test article formulation
- Catheters for serial blood sampling
- LC-MS/MS for bioanalysis
Method:
- Study Design: Use a crossover design where each animal serves as its own control. Randomize the order of treatments.
- Fasted Arm: Fast animals overnight (e.g., 12-16 hours) prior to dosing. Administer the test compound and continue fasting for 4 hours post-dose.
- Fed Arm: Fast animals overnight, then provide a controlled high-fat (or standard) meal shortly before (e.g., 30 min) dosing. Allow access to food immediately after dosing.
- PK Sampling: Collect serial blood samples at pre-defined time points after administration in both arms.
- Bioanalysis & PK Analysis: Determine plasma concentration-time profiles and calculate key PK parameters (Cmax, Tmax, AUC). A significant increase in AUC and Cmax in the fed state suggests a positive food effect, often seen with lipophilic compounds.
Research Reagent Solutions
Table: Essential Materials for Bioavailability Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Caco-2 Cell Line | An in vitro model of the human intestinal epithelium for permeability screening [94]. | Predicting human fractional absorption (FAbs) during lead optimization. |
| Madin-Darby Canine Kidney (MDCK) Cells | An alternative, faster-growing cell line for permeability assessment [94]. | High-throughput ranking of compound permeability. |
| Rat or Mouse In Situ Intestinal Perfusion Model | A more advanced model that maintains intestinal physiology and blood flow [94]. | Obtaining more accurate regional absorption and permeability data. |
| Hydrophilic-Lipophilic Balanced (HLB) SPE Sorbent | A solid-phase extraction sorbent for cleaning up complex biological samples (plasma, urine) prior to analysis [97]. | Reducing matrix effects in LC-MS/MS bioanalysis, improving sensitivity and accuracy. |
| PEG 400 & Polysorbate 80 | Common pharmaceutical solvents and surfactants for creating solution dosing vehicles [94]. | Enhancing the solubility of poorly water-soluble compounds in preclinical PK studies. |
| Biorelevant Media (e.g., FaSSIF/FeSSIF) | Simulated intestinal fluids that mimic the fasting and fed state composition. | In vitro dissolution testing to predict in vivo performance and food effects. |
Validation and Application: Bioequivalence, Comparative Toxicity, and Regulatory Acceptance
Frequently Asked Questions (FAQs)
1. What does the "80/125 rule" for bioequivalence actually mean? It is a common misunderstanding that a generic drug's active ingredient can vary between 80% and 125% of the brand-name drug. The reality is more rigorous. The rule stipulates that the 90% confidence interval for the ratio of the generic (test) drug's key pharmacokinetic parameters (AUC and Cmax) to the brand-name (reference) drug must fall entirely within the 80% to 125% range [98]. This ensures that the entire range of probable difference is within clinically acceptable limits.
2. Why is a 90% confidence interval used and not just the mean value? Using the 90% confidence interval, rather than a simple comparison of means, accounts for variability in the study data. It provides a statistical assurance that the true difference between the two formulations is within the acceptance range in 90% of cases, offering a much more robust guarantee of equivalence than a point estimate alone [98] [99].
3. My study failed bioequivalence. Could high subject variability be the cause? Yes, high intrasubject variability is a common cause of bioequivalence study failure, even if the mean values for the test and reference products are very similar. When variability is high, the confidence interval widens, making it more difficult to fit entirely within the 80-125% bounds. In such cases, a study with a larger sample size may be required to demonstrate equivalence [99].
4. Where did the specific limits of 80% and 125% come from? The limits are based on a clinical judgment by regulators that a difference in systemic drug exposure of more than 20% could be clinically significant. The asymmetrical range arises because the statistical testing is performed on log-transformed pharmacokinetic data, which typically follows a normal distribution. On a log scale, a ±20% difference is symmetrical: the natural log of 0.80 (80%) is -0.223 and the natural log of 1.25 (125%) is +0.223 [100].
5. Are these criteria applied globally? Yes, the 80-125% criterion, with the 90% confidence interval, is a globally harmonized standard for bioequivalence assessment. The ICH M13A guideline, which came into effect in January 2025, further solidifies this international acceptance for immediate-release solid oral dosage forms [101].
Troubleshooting Guides
Problem: Wide Confidence Intervals in Study Data
Potential Causes and Solutions:
- Cause 1: High Intrasubject Variability. This is the most common cause of wide confidence intervals.
- Solution: Perform a robust pilot study to estimate the coefficient of variation (CV) for your drug. Use this data to perform a proper sample size calculation before initiating the main study. The statistical assurance method, which integrates power over a distribution of potential T/R-ratios, can be a more comprehensive approach for sample size determination [99].
- Cause 2: Outliers in Pharmacokinetic Data.
- Solution: Implement strict inclusion/exclusion criteria and standardized procedures during the clinical phase. Pre-define in your statistical analysis plan how potential outliers will be handled, in line with regulatory guidelines [102].
- Cause 3: Inadequate Analytical Method.
- Solution: Validate your bioanalytical method (e.g., LC-MS/MS) per ICH guidelines to ensure precision and accuracy. A poorly performing method adds unwanted variability to your PK parameter estimates.
Problem: Failure to Meet Cmax Criteria Specifically
Potential Causes and Solutions:
- Cause: Formulation Differences Affecting Drug Release Rate.
- Solution: Reformulate the test product to better match the in vitro dissolution profile of the reference product. Utilize quality-by-design (QbD) principles to understand the impact of excipients and manufacturing processes on dissolution and absorption rate.
Quantitative Data and Acceptance Ranges
The following table outlines common acceptance ranges for different types of comparative clinical studies. The principle remains the same: the 90% confidence interval for the ratio of the means must fall within the specified limits [100].
| Study Purpose | Clinical Range | Acceptance Range | Natural Log (ln) Difference |
|---|---|---|---|
| Standard Bioequivalence | ± 20% | 80% – 125% | ± 0.223 |
| Highly Variable Drugs* | ± 30% | 70% – 143% | ± 0.357 |
| Wide Therapeutic Index | ± 50% | 50% – 200% | ± 0.693 |
*Note: Some regulatory agencies allow a widened acceptance range for drugs with known high variability.
Detailed Experimental Protocol: A Standard Two-Treatment, Two-Period Crossover Study
This is the most common design for establishing bioequivalence for immediate-release oral dosage forms.
1. Study Design:
- Type: Randomized, two-sequence, two-period, single-dose crossover study [98].
- Washout Period: Must be sufficient (typically >5 half-lives of the drug) to ensure no carry-over effect from the first period to the second.
2. Subject Selection:
- Number: Determined by a sample size calculation based on intra-subject CV and expected T/R-ratio, often using statistical assurance methods [99].
- Criteria: Healthy volunteers, typically 18-55 years, with normal clinical and laboratory findings.
3. Procedures:
- Dosing: After an overnight fast, subjects receive either the test or reference formulation with 240 mL of water.
- Blood Sampling: Serial blood samples are collected pre-dose and at multiple time points post-dose to adequately characterize the concentration-time profile.
- Sample Analysis: Plasma samples are analyzed using a fully validated bioanalytical method (e.g., HPLC, UPLC-MS/MS).
4. Data Analysis:
- Pharmacokinetic Parameters: The following parameters are calculated for each subject in each period:
- AUC~0-t~: Area under the concentration-time curve from zero to the last measurable concentration, calculated using the linear trapezoidal rule.
- AUC~0-∞~: Area under the curve from zero to infinity.
- C~max~: Maximum observed concentration.
- Statistical Analysis:
- An ANOVA is performed on the log-transformed AUC and C~max~ data.
- The 90% confidence intervals for the ratio of geometric means (Test/Reference) for AUC and C~max~ are calculated.
- Bioequivalence Conclusion: If the 90% CIs for both AUC and C~max~ are entirely within the 80-125% range, bioequivalence is concluded [98] [101].
Visualizing the Bioequivalence Study Workflow
The following diagram illustrates the logical flow and decision points in a standard bioequivalence study.
Bioequivalence Study Decision Flow
The Scientist's Toolkit: Essential Reagents and Materials
| Item | Function in Bioequivalence Studies |
|---|---|
| Validated Bioanalytical Method (e.g., LC-MS/MS) | Quantifies the concentration of the active drug and/or its metabolites in biological fluids (e.g., plasma) with high specificity, accuracy, and precision. This is the cornerstone of generating reliable PK data. |
| Certified Reference Standards | Highly characterized samples of the active pharmaceutical ingredient (API) with known purity and identity. Essential for calibrating analytical instruments and ensuring the accuracy of concentration measurements. |
| Stable Isotope-Labeled Internal Standard | Used in mass spectrometry-based assays to correct for sample preparation losses and matrix effects, significantly improving the accuracy and reproducibility of the analytical results. |
| Control Matrix (e.g., Drug-Free Plasma) | The biological fluid without the analyte of interest. Used to prepare calibration standards and quality control (QC) samples for the analytical run. |
| Chromatography Supplies | Includes HPLC/UPLC columns, mobile phase solvents, and solvents for sample preparation. Critical for separating the analyte from other components in the biological matrix before detection. |
In the context of bioavailability and toxicity testing research, selecting an appropriate study design is paramount for generating reliable, interpretable, and regulatory-acceptable data. Bioavailability, which assesses the rate and extent of absorption of an active compound into the bloodstream, is a cornerstone of pharmaceutical development, particularly for generic drugs where demonstrating bioequivalence is required. Two of the most critical experimental designs used in this field are the crossover design and the parallel design. Each has distinct advantages, limitations, and ideal use cases. This technical support guide provides a detailed comparison of these designs, complete with troubleshooting advice and frequently asked questions, to help researchers and scientists make informed decisions in their preclinical and clinical study planning. The fundamental difference lies in how subjects are exposed to treatments: in a crossover design, each subject receives multiple treatments in sequence, while in a parallel design, each subject receives only one treatment [103] [104] [105].
Fundamental Concepts and Definitions
Crossover Design
In a crossover design, each experimental unit (e.g., a human volunteer or an animal) receives different treatments during different time periods. The order of treatment administration is randomized. The most basic form is the 2x2 crossover design, where subjects are randomly allocated to one of two sequences: either receiving treatment A first, followed by treatment B after a washout period, or vice versa (B followed by A) [103] [104]. This design is highly efficient because it uses each subject as their own control.
Parallel Design
In a parallel design, subjects are randomized to receive one of the treatments under investigation and remain on that treatment throughout the duration of the study. The comparison of treatment effects is therefore made between different groups of subjects [103] [106]. This design is simpler to execute and is necessary when treatments have permanent effects.
Direct Comparison: Advantages and Disadvantages
The choice between a crossover and a parallel design involves a trade-off between statistical efficiency and practical feasibility. The table below summarizes the key advantages and disadvantages of each design.
Table 1: Advantages and Disadvantages of Crossover vs. Parallel Designs
| Aspect | Crossover Design | Parallel Design |
|---|---|---|
| Statistical Power | High power and statistical efficiency; requires fewer subjects to detect a given effect size [103] [106]. | Lower statistical power per subject; generally requires a larger sample size for the same power [106]. |
| Control of Variability | Removes inter-subject variability as each subject serves as their own control [103] [104]. | More susceptible to inter-subject variability, which can obscure treatment effects [103]. |
| Suitability for Conditions | Only suitable for chronic, stable conditions where the disease state returns to baseline (e.g., asthma, hypertension) [104]. | Suitable for a wider range of conditions, including acute diseases and treatments that are curative [104]. |
| Carryover Effects | Highly susceptible to carryover effects, which can bias results if the washout period is inadequate [103] [104]. | Not susceptible to carryover effects, as each subject receives only one treatment [103]. |
| Study Duration & Dropouts | Typically longer per subject, which can increase the risk of dropouts; missing data is more problematic to handle [103]. | Shorter duration per subject; lower risk of dropouts due to study length [103]. |
| Resource & Ethical Burden | More complex logistics; burden on subjects is higher as all treatments are applied to each one [103]. | Logistically simpler; lower burden on each individual subject [103] [105]. |
Quantitative Performance Comparison
A direct analysis based on a large study in nonhuman primates (NHPs) quantitatively compared the sensitivity of these two designs for QTc interval assessment. The study's large size (n=48) allowed it to be analyzed both as a crossover and a parallel design, keeping all other experimental conditions identical. The key metric for sensitivity was the Minimal Detectable Difference (MDD), which is the smallest true treatment effect a study design can detect with a given power. A smaller MDD indicates higher sensitivity [106].
Table 2: Sensitivity Comparison for QTc Assessment based on NHP Study (n=48)
| Study Design | Statistical Model | Minimal Detectable Difference (MDD) | Implications |
|---|---|---|---|
| Parallel Design | Treatment + Baseline | 12.7 ms (for n=6/group) | Reasonable sensitivity, may require higher exposures for integrated risk assessment [106]. |
| Crossover Design | Treatment + Individual Animal ID (ID) | 12.2 ms (for n=4); 8 ms (for n=8) | Higher sensitivity, especially with larger n; ideal when detection of small effects is critical [106]. |
This empirical data demonstrates that for the same endpoint, the crossover design provides greater sensitivity with fewer subjects. For example, a crossover design with 8 animals (n=8) can detect a difference of 8 ms, whereas a parallel design with a total of 12 animals (n=6 per group) can only detect a difference of 12.7 ms [106].
Experimental Protocols and Methodologies
Protocol for a Standard 2x2 Crossover Bioequivalence Study
This protocol is commonly used for comparing the bioavailability of two formulations of the same drug.
- Step 1: Subject Selection and Randomization. Enroll healthy volunteers or animal subjects that meet the inclusion criteria. The population should be as homogeneous as possible to minimize sequence effects. Randomly assign subjects to either sequence AB (Treatment A first, then B) or sequence BA (Treatment B first, then A) [103] [104].
- Step 2: First Period Dosing. After a baseline assessment, administer the assigned treatment (A for sequence AB, B for sequence BA) to all subjects. The formulation (test or reference) should be administered under standardized conditions (e.g., fasting) [103].
- Step 3: Pharmacokinetic (PK) Sampling. Collect serial blood samples over a period sufficient to characterize the complete concentration-time profile of the drug (e.g., 2-3 times the elimination half-life). Key PK parameters like AUC (Area Under the Curve) and Cmax (maximum concentration) will be derived from this data [107].
- Step 4: Washout Period. Implement a washout period of sufficient length between the two treatment periods. This period, typically 5 or more times the half-life of the drug, is critical to ensure the effects of the first treatment have subsided before the second period begins, thereby minimizing carryover effects [103] [104].
- Step 5: Second Period Dosing and PK Sampling. Cross over the treatments. Subjects in sequence AB now receive treatment B, and those in sequence BA receive treatment A. Repeat the same PK sampling schedule as in the first period [103].
- Step 6: Data Analysis. Use a linear mixed-effects model to analyze the PK parameters. The model should account for fixed effects (sequence, period, and treatment) and random effects (subject within sequence). Bioequivalence is concluded if the 90% confidence interval for the geometric mean ratio (Test/Reference) of AUC and Cmax falls entirely within the acceptance range of 80.00% to 125.00% [103] [107].
Protocol for a Parallel Group Toxicity Study
This design is often used in toxicology or for compounds with long half-lives.
- Step 1: Group Formation and Randomization. Enroll subjects and randomize them into separate, independent groups. The number of groups equals the number of treatments being compared (e.g., Vehicle control, Low dose, Mid dose, High dose) [106] [108].
- Step 2: Baseline Measurements. Record baseline measurements for all key endpoints (e.g., clinical observations, clinical pathology, ECG for QTc) for all subjects [106].
- Step 3: Treatment Administration. Administer the respective treatment to each group. Dosing continues for the pre-defined study duration, which can range from a single dose to repeated doses over weeks or months, depending on the study objectives [108].
- Step 4: In-life and Terminal Measurements. Throughout the study, collect in-life data (e.g., food consumption, body weight, clinical signs). At the end of the dosing period and/or at scheduled interim timepoints, collect terminal endpoints such as detailed clinical pathology, histopathology, and toxicokinetic blood samples to assess exposure [108].
- Step 5: Data Analysis. Compare the outcome measures between the treatment groups and the control group using statistical models appropriate for between-group comparisons (e.g., ANOVA). The model may include baseline values as a covariate to improve precision, especially in studies with higher inter-subject variability [106].
Troubleshooting Common Experimental Issues
FAQ 1: How can I effectively manage and test for carryover effects in my crossover study?
Carryover effects are a major threat to the validity of crossover studies.
- Prevention is Key: The most effective strategy is to prevent carryover effects by designing an adequate washout period. For drug studies, this should be based on pharmacokinetic data, typically 3-5 times the terminal half-life of the drug to ensure it is cleared from the body [103] [104].
- Statistical Testing: If a washout period cannot be made sufficiently long, a statistical test for differential carryover can be attempted using a general linear model. However, this test has low power and is correlated with the test for treatment effects, making interpretation difficult [103] [104].
- Design Solution: If differential carryover is a significant concern, consider using a more complex design (e.g., a Balaam's design or a 4-period design with two sequences) where the carryover effect is not aliased (confounded) with the direct treatment effect [104].
FAQ 2: My study failed to show a significant effect. Was my sample size too small?
This is a common issue that can stem from both crossover and parallel designs.
- A Priori Calculation: Always perform a sample size calculation before starting the study. For crossover designs, this depends on the within-subject variability, the desired power (typically 80-90%), and the bioequivalence limits (80-125%). For parallel designs, it depends on the between-subject variability [107].
- High Variability: If a study with a seemingly adequate sample size fails, high variability might be the culprit. For future studies on highly variable drugs, consider using replicate crossover designs (e.g., a 2x4 design where each subject receives each treatment twice). These designs provide a more precise estimate of within-subject variability for both formulations and can be advantageous for demonstrating bioequivalence for highly variable drugs [107].
- Parallel Design Inefficiency: If a parallel design failed, switching to a crossover design (if ethically and scientifically justified) could provide the necessary power with a similar or even smaller number of subjects, as it controls for the largest source of variability—the differences between subjects [103] [106].
FAQ 3: When is a parallel design absolutely necessary over a crossover design?
A crossover design is not universally applicable. A parallel design is mandatory in the following situations:
- The treatment is curative: If the first treatment cures the disease (e.g., an antibiotic for an infection), there is no condition to treat in the second period [104].
- The treatment has an irreversible or permanent effect: This includes surgeries, some gene therapies, or treatments that cause permanent physiological changes [104] [105].
- The disease is acute or rapidly changing: The condition must be stable throughout the study for the comparison to be valid [103].
- The drug has an extremely long half-life: Making a washout period logistically or ethically impractical (e.g., very long-term toxicity studies) [106] [108].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials for Bioavailability and Toxicity Study Conduct
| Item/Category | Function in the Study | Specific Examples & Considerations |
|---|---|---|
| Biorelevant Dissolution Media | To simulate in vivo conditions of the gastrointestinal tract for in vitro dissolution testing, providing better in vitro-in vivo correlation (IVIVC) [34]. | FaSSGF (Fasted State Simulated Gastric Fluid), FeSSGF (Fed State), FaSSIF (Intestinal Fluid), FeSSIF. These contain surfactants and buffers to mimic fed and fasted states [34]. |
| In Vitro/Ex Vivo Permeability Models | To predict the absorption potential of a drug substance through biological barriers. | PAMPA (Parallel Artificial Membrane Permeability Assay) for passive transcellular permeability; Caco-2 cell cultures; using excised animal or human tissues (ex vivo) [34]. |
| Formulation Vehicles | To deliver the active pharmaceutical ingredient (API) in a stable and bioavailable form, especially for poorly soluble compounds. | Lipid-based formulations (LBFs), co-solvents, suspensions. Note: Lipid formulations may require in vitro lipolysis tests to assess precipitation risk upon digestion [34]. |
| Analytical Standards & Reagents | For the accurate and precise quantification of drug concentrations in biological matrices (e.g., plasma, serum) for pharmacokinetic analysis. | High-purity reference standards of the API and its metabolites, stable isotope-labeled internal standards, HPLC-grade solvents, specific antibodies for immunoassays [103] [108]. |
| Telemetry Implants & ECG Analysis Systems | For continuous, high-quality cardiovascular safety monitoring in conscious, freely moving animals, a key component of safety pharmacology. | Implantable telemetry devices for measuring blood pressure, heart rate, and ECG; jacketed external telemetry; automated software for QTc analysis [106]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
FAQ 1: Why do my nanoparticles show high toxicity in vitro but poor efficacy in vivo? This discrepancy often arises from poor bioavailability. Nanoparticles may fail to reach their target site in vivo due to biological barriers, rapid clearance, or aggregation. The enhanced permeability and retention (EPR) effect in tumors can be highly variable, and nanoparticles must circulate long enough to accumulate [109]. Solution: Focus on optimizing physicochemical parameters like size, surface charge, and functionalization to improve biodistribution and reduce off-target accumulation [110] [109].
FAQ 2: How does nanoparticle surface charge influence toxicity and biodistribution? Surface charge critically affects protein adsorption, cellular uptake, and immune recognition. Cationic surfaces often show higher cytotoxicity due to stronger interactions with negatively charged cell membranes, leading to greater membrane disruption and inflammatory responses [110] [53]. Solution: For reduced toxicity and longer circulation, aim for a neutral or slightly negative surface charge. Pegylation can shield surface charge and improve stealth properties [109] [111].
FAQ 3: What is the impact of nanoparticle size on organ-specific biodistribution? Size directly determines which physiological barriers a nanoparticle can cross and its organ accumulation. Smaller particles (<10 nm) are rapidly cleared by renal filtration, while larger particles (>100 nm) are more readily taken up by the liver and spleen [110] [109]. Solution: For most therapeutic applications targeting solid tumors, a size range of 20-150 nm is optimal for leveraging the EPR effect and avoiding rapid clearance [109].
FAQ 4: How does the manufacturing method impact nanoparticle reproducibility and toxicity? The preparation technique (e.g., microfluidics vs. bulk mixing) directly influences critical quality attributes like size, polydispersity, and internal structure, which in turn govern biological performance [112] [111]. Solution: Use controlled microfluidic mixing for higher batch-to-batch consistency. Characterize multiple structural parameters beyond just size, as internal architecture correlates with delivery efficiency [112].
FAQ 5: Why is characterizing nanoparticle shape important for toxicity assessment? Shape affects cellular internalization, flow properties, and biodistribution. Spherical particles are typically internalized more slowly than high-aspect-ratio particles like rods, which can influence both toxicity and efficacy [110]. Solution: Employ multiple orthogonal characterization techniques (e.g., SAXS, FFF-MALS, SV-AUC) to fully understand shape and internal structure, as these properties are not revealed by dynamic light scattering alone [112].
Experimental Protocols for Bioavailability and Toxicity Assessment
Protocol 1: In Vivo Biodistribution and Tolerability Study
Objective: To evaluate organ-specific accumulation, clearance pathways, and systemic tolerability of nanoparticle formulations.
Materials:
- Test nanoparticles (e.g., nanodiamonds, gold nanoparticles, quantum dot nanocarbons)
- Animal model (e.g., C57BL/6 mice)
- Flow cytometer with appropriate antibodies (e.g., anti-CD69, anti-CD25)
- ELISA kits for cytokine analysis (e.g., IL-6, TNF-α)
- Tissue digestion system and elemental analysis equipment (if applicable)
Methodology:
- Dosing: Administer nanoparticles intravenously at multiple dose levels (e.g., 5, 10, 20, and 40 mg/kg) to establish dose-response relationships [113].
- Sample Collection: Euthanize animals at predetermined time points (e.g., 2, 24, and 96 hours). Collect blood, liver, spleen, kidney, heart, and lung tissues [113].
- Immune Response Analysis:
- Biodistribution Quantification:
- Digest tissue samples and quantify nanoparticle accumulation using appropriate techniques (e.g., elemental analysis, fluorescence tracking) [113].
- Calculate organ-specific accumulation as percentage of administered dose per gram of tissue.
- Data Interpretation: Correlate biodistribution patterns with observed immune responses and clinical observations to establish therapeutic windows.
Protocol 2: Mechanistic Toxicity Profiling via Oxidative Stress Pathways
Objective: To investigate nanoparticle-induced oxidative stress as a key mechanism of toxicity.
Materials:
- Cell culture model (e.g., primary macrophages, endothelial cells)
- Nanoparticle suspensions in appropriate vehicles
- ROS detection probes (e.g., DCFH-DA, MitoSOX)
- Apoptosis/necrosis detection kits
- Glutathione assay kit
- Mitochondrial membrane potential assay
Methodology:
- Dose Optimization: Conduct preliminary viability assays (MTT, Alamar Blue) to establish sublethal and lethal concentration ranges [53].
- ROS Measurement: Treat cells with nanoparticles and measure intracellular ROS production at multiple time points using fluorescent probes. Include positive (e.g., Hâ‚‚Oâ‚‚) and negative controls [53].
- Antioxidant Defense Assessment: Measure glutathione depletion and antioxidant enzyme activities (e.g., SOD, catalase) to evaluate compensatory cellular responses [110] [53].
- Mitochondrial Function: Assess mitochondrial membrane potential (JC-1 assay) and ATP production to determine metabolic impacts [53].
- Cell Death Mechanisms: Distinguish between apoptosis and necrosis using Annexin V/PI staining and caspase activation assays [53].
- Data Analysis: Correlate ROS generation with mitochondrial dysfunction and cell death to establish causal relationships between nanoparticle properties and toxicity mechanisms.
Comparative Toxicity and Bioavailability Data
Table 1: Immune Response Profiles of Different Nanoparticles
| Nanoparticle Type | CD69 Expression (CD8+ T cells) | CD25 Expression | IL-6 Elevation | TNF-α Elevation | Primary T-cell Impact |
|---|---|---|---|---|---|
| Unconjugated Nanodiamonds | 0.12 ± 0.09 | Not elevated | Minimal | Minimal | Lowest activation (40.70% ± 8.10 total T cells) |
| Nanobody-Conjugated Nanodiamonds | Moderate | 0.09 ± 0.04 | Significant at 2 hours | Significant at 2 hours | Highest activation (49.10% ± 6.99 total T cells) |
| Gold Nanoparticles | 0.40 ± 0.16 | Elevated | Significant | Significant | Strong memory T cell activation |
| Quantum Dot Nanocarbons | Elevated | 0.23 ± 0.04 | Moderate | Moderate | Significant memory T cell activation |
Data adapted from Alexander & Leong (2025) [113]
Table 2: Organ-Specific Biodistribution Patterns (% Injected Dose/Gram)
| Nanoparticle Type | Heart | Left Lung | Kidney | Liver | Spleen | Blood (96h) |
|---|---|---|---|---|---|---|
| Nanodiamonds | Primary accumulation | Low | Moderate | Moderate (≈60%) | High | Cleared |
| Gold Nanoparticles | Low | Primary accumulation | Low | Moderate | High | Cleared |
| Quantum Dot Nanocarbons | Persistent | Low | Primary accumulation | High | Moderate | Persistent |
Data summarized from Alexander & Leong (2025) [113]
Table 3: Influence of Physicochemical Properties on Toxicity and Bioavailability
| Parameter | Optimal Range for Reduced Toxicity | Impact on Bioavailability | Key Toxicity Mechanisms |
|---|---|---|---|
| Size | 20-100 nm | <10 nm: renal clearance>200 nm: RES uptake | Small sizes: membrane penetrationLarge sizes: embolism risk |
| Surface Charge | Neutral to slightly negative (-10 to +10 mV) | Cationic: increased non-specific uptakeAnionic: prolonged circulation | Cationic: membrane disruption, ROS |
| Shape | Spherical vs. high-aspect-ratio | Rods: different internalization kineticsSpheres: more predictable distribution | High-aspect-ratio: frustrated phagocytosis |
| Surface Chemistry | PEGylated, hydrophilic | Hydrophobic: protein adsorption, opsonization | Reactive surfaces: ROS, protein denaturation |
Data synthesized from multiple sources [110] [109] [53]
Experimental Workflows and Signaling Pathways
Nanoparticle Toxicity Signaling Pathway
Toxicity Testing Experimental Workflow
Research Reagent Solutions
Essential Materials for Nanoparticle Toxicity and Bioavailability Studies
| Reagent Category | Specific Examples | Function in Research | Application Notes |
|---|---|---|---|
| Lipid Nanoparticle Components | Ionizable lipids (e.g., DLin-MC3-DMA), PEGylated lipids (e.g., Brij S20), helper lipids (e.g., Lipoid S100) | Form stable, biocompatible delivery systems | Helper lipids enhance stability and drug loading; PEG length affects circulation time [114] [111] |
| Metallic Nanoparticles | Gold nanoparticles, silver nanoparticles, iron oxide nanoparticles | Imaging, thermal therapy, diagnostic applications | Size and shape critically influence toxicity profiles; surface coating reduces aggregation [110] [113] |
| Carbon-Based Nanomaterials | Nanodiamonds, quantum dot nanocarbons, carbon nanotubes | Drug delivery, bioimaging, tissue engineering | Nanodiamonds show favorable tolerability; quantum dots require careful toxicity screening [113] |
| Polymer-Based Nanoparticles | PLGA, chitosan, dendrimers | Controlled release, targeted delivery | Biodegradability reduces long-term toxicity concerns; surface functionalization enables targeting [110] |
| Characterization Reagents | Dynamic light scattering standards, zeta potential standards, fluorescent dyes (e.g., DiO, DiI) | Quality control, tracking, biodistribution studies | Essential for establishing reproducible formulation parameters [112] [111] |
| Toxicity Assay Kits | MTT, LDH, ROS detection, caspase activity, cytokine ELISA | Mechanism-specific toxicity assessment | Multiple assays required for comprehensive safety profiling [113] [53] |
This technical support resource addresses key experimental challenges in bioavailability research for two critical materials: alumina nanoparticles (toxicological subjects) and resveratrol nanoparticles (therapeutic agents). Understanding their distinct behaviors in nano-form versus traditional form is paramount for accurate toxicity testing and drug development.
Bioavailability & Toxicity: Core Concepts FAQ
Q1: What is the fundamental difference in bioavailability between traditional and nano-form materials?
The key difference lies in their bioavailability - the proportion and rate at which a substance enters systemic circulation to access its site of action. Nano-forms fundamentally alter this through:
- Increased Surface Area to Volume Ratio: Nanoparticles have dramatically increased surface area, which enhances their solubility, reactivity, and interaction with biological systems [115] [116].
- Altered Uptake and Distribution: Their small size allows them to cross biological barriers that traditional forms cannot, leading to unique distribution patterns in tissues and organs [115] [117].
- Modified Clearance: Nanoparticles can evade normal clearance mechanisms, leading to prolonged systemic presence and potential accumulation [116] [117].
Q2: Why does the low oral bioavailability of traditional resveratrol limit its therapeutic potential, and how do nano-formulations address this?
Traditional resveratrol suffers from several pharmacokinetic limitations that nano-formulations are designed to overcome.
| Limitation Factor | Traditional Resveratrol | Resveratrol Nano-Formulations |
|---|---|---|
| Aqueous Solubility | Very low (~0.03 mg/mL) [118] | Enhanced via encapsulation (e.g., in polymeric NPs, lipid carriers) [115] |
| Systemic Bioavailability | Almost zero after oral administration [118] | Enhanced tumor accumulation and controlled release [115] |
| Chemical Stability | Low; susceptible to environmental conditions [119] | Protected within nanoparticle matrix; improved photothermal stability [119] |
| Metabolism | Rapid metabolism and conjugation in intestine/liver [120] | Metabolism bypassed or delayed via targeted delivery [115] |
Nano-formulations like polymeric nanoparticles, solid lipid nanoparticles, and metal-polyphenol supramolecular coatings directly counter these limitations by protecting resveratrol, enhancing its absorption, and facilitating targeted delivery to specific tissues [115] [119].
Q3: What are the primary toxicological concerns associated with alumina nanoparticles compared to their traditional forms?
While bulk alumina is generally considered inert, alumina nanoparticles (Al₂O₃ NPs) exhibit unique toxicological profiles due to their nanoscale properties.
| Toxicological Aspect | Traditional/Bulk Alumina | Alumina Nanoparticles (Al₂O₃ NPs) |
|---|---|---|
| Pulmonary Inflammation | Limited evidence at low exposures [116] | Significant inflammatory response; increased neutrophils, IL-8, TNF-α in BALF [116] |
| Systemic Distribution & Organ Accumulation | Limited absorption and distribution [117] | Rapid absorption; distributed to liver, kidney, spleen, and brain [117] |
| Neurotoxicity | Not typically reported | Learning/memory impairment; oxidative stress in brain [121] |
| Persistence & Long-Term Effects | Cleared more readily | Highly persistent in organs (e.g., half-life in brain up to 150 days) [117] |
The small size and high reactivity of Al₂O₃ NPs can trigger oxidative stress, inflammation, and, with chronic exposure, may lead to more severe outcomes like pulmonary fibrosis and neurotoxicity [116] [121].
Experimental Protocols & Methodologies
Protocol 1: Assessing Oral Bioavailability and Systemic Distribution of Nanoparticles
This protocol is adapted from studies on alumina nanoparticles [117] and can be applied to assess the bioavailability of various nano-formulated substances.
1. Objective: To quantify the absorption and organ-specific distribution of nanoparticles following oral administration.
2. Materials:
- Test nanoparticles (e.g., Al₂O₃ NPs, Resveratrol-loaded NPs)
- Animal model (e.g., Sprague Dawley rats)
- Gavage equipment
- ICP-MS (Inductively Coupled Plasma Mass Spectrometry) system
- Microwave-assisted digestion system
3. Methodology:
- Dosing: Administer a precise dose of nanoparticles to animals via oral gavage. Include control groups (e.g., vehicle control, ionic/bulk form).
- Tissue Collection: After a predetermined period (e.g., 3 days), euthanize animals and collect organs of interest (e.g., liver, spleen, kidney, brain, intestines).
- Sample Digestion: Digest weighed tissue samples using a validated microwave-assisted acid digestion protocol to dissolve nanoparticles and release the target element (e.g., Al for alumina, or the nanoparticle core material).
- ICP-MS Analysis:
- Critical Step - Matrix-Matched Calibration: Prepare calibration standards in a blank matrix of each homogenized organ type. This corrects for matrix suppression effects during ICP-MS analysis, which is crucial for accurate quantification [117].
- Analyze digested samples and calculate the concentration of the target element in each organ (e.g., µg of Al per gram of tissue).
4. Data Interpretation: Compare organ burdens between nano-form and traditional form treatments to evaluate differences in bioavailability and distribution patterns.
Protocol 2: Evaluating the Enhanced Efficacy of Nano-Formulated Resveratrol
This protocol outlines a method to test the superior performance of resveratrol nanoparticles [115] [119].
1. Objective: To demonstrate the improved antioxidant activity and controlled release of resveratrol from nanoparticle formulations.
2. Materials:
- Resveratrol nanoparticles (e.g., composite RES NPs with metal-polyphenol coating)
- Free (traditional) resveratrol
- In vitro simulated digestion model (e.g., simulating gastric and intestinal fluids)
- Cell culture models (e.g., cancer cell lines for efficacy testing)
- Assays for antioxidant activity (e.g., DPPH assay) and drug release (HPLC)
3. Methodology:
- Stability & Antioxidant Testing:
- Expose both free resveratrol and resveratrol nanoparticles to stress conditions (e.g., light, heat).
- Measure and compare the remaining antioxidant capacity using standard assays.
- In Vitro Release and Digestion:
- Subject resveratrol nanoparticles to a simulated gastrointestinal tract environment using biorelevant media (e.g., FaSSGF, FaSSIF, FeSSIF) [34].
- Sample the release medium at timed intervals and use HPLC to quantify the amount of resveratrol released, demonstrating controlled release profiles.
- Cellular Efficacy:
- Treat relevant cell lines (e.g., cancer cells) with both free resveratrol and resveratrol nanoparticles across a range of concentrations.
- Assess cytotoxicity, apoptosis, and markers of target engagement (e.g., expression of SIRT1 or apoptotic proteins) to establish enhanced efficacy at lower doses.
4. Data Interpretation: Nano-formulated resveratrol is expected to show superior stability, controlled release kinetics, and greater potency in cellular assays compared to the free form.
The following workflow visualizes the key experimental and regulatory pathway for assessing nanoparticle bioavailability and safety, integrating the protocols above.
Experimental and Regulatory Workflow for Nanoparticle Assessment
The Scientist's Toolkit: Essential Research Reagents & Materials
This table details key reagents and their functions for conducting the experiments described in this guide.
| Research Reagent / Material | Critical Function in Experimentation |
|---|---|
| Simulated Intestinal Fluids (FaSSIF/FeSSIF) | Biorelevant dissolution media that mimic the fasted and fed states of the human GI tract for predictive in vitro release studies [34]. |
| ICP-MS with Matrix-Matched Calibration | Gold-standard for quantifying metal-based nanoparticle (e.g., Al₂O₃) concentration in tissues; matrix-matching is critical for accuracy [117]. |
| Polymeric/Lipid Nanocarriers | Delivery systems (e.g., PLGA, solid lipid NPs) used to encapsulate resveratrol, enhancing its solubility, stability, and targeted delivery [115]. |
| Metal-Polyphenol Supramolecules | Coating materials (e.g., Catechin + Fe³âº/Ca²âº) used to stabilize resveratrol nanoparticles and enhance their antioxidant properties [119]. |
| Transwell Cell Culture Systems | In vitro models (e.g., Caco-2 monocultures or co-cultures) used to study nanoparticle permeability and transport across biological barriers [34]. |
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or inaccurate quantification of nanoparticle uptake in tissues.
- Potential Cause: Matrix suppression effects during ICP-MS analysis.
- Solution: Implement a matrix-matched calibration for each organ type. Prepare calibration standards in a blank digestate of the target tissue to correct for signal suppression and ensure accurate quantification [117].
Challenge 2: Rapid precipitation and instability of resveratrol during in vitro dissolution testing.
- Potential Cause: The transfer from gastric to intestinal conditions can cause supersaturation and subsequent precipitation of resveratrol.
- Solution: Use a transfer model dissolution apparatus. This system connects gastric and intestinal compartments with a peristaltic pump, mimicking the dynamic transition in the GI tract and providing a more realistic assessment of precipitation and release [34].
Challenge 3: Resveratrol nanoparticles degrade or aggregate during storage.
- Potential Cause: Exposure to environmental factors like light and oxygen, or insufficient stabilization.
- Solution: Incorporate stabilizers like metal-polyphenol supramolecular coatings (e.g., using catechin and metal ions). These coatings significantly improve photothermal stability and prevent aggregation, maintaining nanoparticle integrity [119].
Regulatory Considerations for Bioavailability Assessment
According to the U.S. Code of Federal Regulations (21 CFR § 320.24), acceptable methods for measuring bioavailability or establishing bioequivalence are listed in descending order of accuracy, sensitivity, and reproducibility [122]:
- In vivo testing in humans with measurement of the active moiety in blood/plasma.
- In vitro tests that are predictive of human in vivo bioavailability data.
- In vivo testing in humans with measurement of urinary excretion.
- In vivo testing in humans with measurement of an acute pharmacological effect.
- Well-controlled clinical trials that establish safety and effectiveness.
For nanoparticle research, correlating in vitro data (e.g., dissolution, permeability) with in vivo outcomes is a powerful strategy for regulatory acceptance [34] [122].
Bioavailability is defined as the rate and extent to which the active drug ingredient or moiety is absorbed from a drug product and becomes available at the site of drug action [123]. In practical terms, it represents the fraction of an administered dose that reaches the systemic circulation unchanged.
Bioequivalence refers to the absence of a significant difference in the rate and extent to which the active ingredient becomes available at the site of drug action when pharmaceutical equivalents or alternatives are administered at the same molar dose under similar conditions [123].
Table 1: Key Definitions
| Term | Definition | Regulatory Reference |
|---|---|---|
| Bioavailability | The rate and extent of drug absorption to the site of action | 21 CFR Part 320.1 [123] |
| Bioequivalence | No significant difference in bioavailability between products | FDA Guidance [102] |
| Therapeutic Equivalence | Same safety and efficacy profile | Fundamental Bioequivalence Assumption [123] |
The Fundamental Bioequivalence Assumption states that if two drug products are shown to be bioequivalent, it is assumed that they will reach the same therapeutic effect or are therapeutically equivalent [123]. This principle forms the foundation for generic drug approval worldwide, allowing reliance on bioavailability measurements as surrogates for clinical outcomes.
Frequently Asked Questions (FAQs)
FAQ 1: What is the Fundamental Bioequivalence Assumption and why is it critical for generic drug development?
The Fundamental Bioequivalence Assumption is the cornerstone principle that allows regulatory agencies to approve generic drugs based on bioavailability studies rather than requiring extensive clinical trials [123]. This assumption states that demonstrating bioequivalence between a generic and reference product is sufficient to predict therapeutic equivalence. The economic impact is substantial—generic drugs typically cost about 20% of brand-name originals, making treatments more accessible [123]. Without this principle, each generic drug would require the same extensive clinical testing as innovative drugs, dramatically increasing development costs and time to market.
FAQ 2: What are the standard regulatory criteria for establishing bioequivalence?
Regulatory agencies worldwide have established specific statistical criteria for bioequivalence assessment. The FDA primarily uses the 80/125 rule, which requires that the 90% confidence interval for the ratio of geometric means (Test/Reference) of primary pharmacokinetic parameters (AUC and Cmax) must fall entirely within the limits of 80% to 125% after log-transformation [123]. The European Medicines Agency (EMA) recommends a similar approach using average bioequivalence (ABE) [124]. These criteria ensure that differences between products are sufficiently small to be clinically insignificant.
Table 2: Bioequivalence Assessment Methods
| Method | Key Characteristics | Primary Use | Limitations |
|---|---|---|---|
| Average Bioequivalence (ABE) | Compares mean values (Test vs Reference) using 90% CI [124] | Standard method in EU [124] | Does not consider between-batch variability [124] |
| Population Bioequivalence (PBE) | Accounts for variance differences between products [124] | Recommended by FDA for some products [124] | Asymmetric formula can be problematic [124] |
| Between-Batch Bioequivalence (BBE) | Incorporates between-batch variability in assessment [124] | Emerging approach for variable products [124] | Not yet widely adopted in regulations [124] |
FAQ 3: How does low oral bioavailability impact toxicity testing for substances like metal salts?
Low oral bioavailability presents significant challenges for toxicity testing and risk assessment. Using aluminum salts as an example, which have oral bioavailability below 1%, applicable doses in toxicity studies are limited by low systemic exposure, making it difficult to induce clear adverse effects that can serve as points of departure for risk characterization [125] [126]. The low systemic doses achieved may be insufficient to overcome background exposures from ubiquitous environmental presence, potentially confounding study results [126]. Furthermore, substances with low bioavailability may exhibit route-specific toxicity patterns, where oral administration shows minimal effects compared to other exposure routes [126].
FAQ 4: When is therapeutic drug monitoring (TDM) necessary for bioavailability assessment?
Therapeutic drug monitoring is particularly valuable for drugs with a narrow therapeutic index, marked pharmacokinetic variability, or difficult-to-monitor target concentrations [127]. TDM involves measuring drug concentrations in biological fluids (typically blood, plasma, or serum) to optimize individual dosage regimens [127] [128]. Key indications include:
- Assessing efficacy when therapeutic effects are difficult to monitor clinically
- Diagnosing toxicity, especially when symptoms mimic disease states
- Evaluating potential drug-drug interactions
- Monitoring patient compliance [127] TDM is most beneficial when there's a well-established relationship between drug concentration and clinical response [128].
Troubleshooting Common Experimental Issues
Problem 1: High Variability in Bioavailability Measurements
Issue: Unacceptable between-batch variability compromising bioequivalence assessment.
Solution: Consider alternative statistical approaches:
- Between-Batch Bioequivalence (BBE): This method specifically accounts for between-batch variability by comparing the mean difference (Reference - Test) to the Reference between-batch variability [124].
- Increased Sample Size: For traditional ABE and PBE methods, increasing sample size can improve test power when variability is high [124].
- Study Design Optimization: Implement rigorous randomization and blocking strategies to minimize confounding factors.
Preventive Measures:
- Standardize manufacturing processes to minimize batch-to-batch variation
- Implement rigorous quality control measures
- Conduct pilot studies to estimate variability for sample size calculations
Problem 2: Confounding Factors in Oral Bioavailability Studies
Issue: Low and variable oral bioavailability due to physicochemical and physiological factors.
Solution:
- Control Gastric Environment: Standardize fasting conditions or use controlled gastric pH modifiers when scientifically justified
- Account for First-Pass Metabolism: Consider population genetics of metabolic enzymes (CYP450 family) that contribute to interindividual variability [129]
- Validate Analytical Methods: Ensure bioanalytical methods can distinguish parent drug from metabolites, especially for drugs with extensive first-pass metabolism [128]
Experimental Protocol:
- Fast subjects for at least 8 hours prior to dosing
- Administer drug with standardized fluid volume (typically 240 mL water)
- Standardize meal timing (e.g., 4 hours post-dose) if non-fasting design is used
- Collect serial blood samples adequate to define absorption and elimination phases
- Analyze samples using validated methods specific for the parent compound
Problem 3: Establishing Correlation Between Bioavailability and Therapeutic Outcome
Issue: Uncertain therapeutic relevance of bioavailability differences.
Solution:
- Implement Therapeutic Drug Monitoring: For drugs with established concentration-response relationships, TDM can bridge bioavailability and therapeutic effect [127]
- Validate Surrogate Endpoints: Establish correlation between pharmacokinetic parameters (AUC, Cmax) and clinical outcomes during drug development
- Consider Pharmacodynamic Measurements: Incorporate direct measures of pharmacological effect when available
Assessment Framework:
Bioavailability to Therapeutic Outcome Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Bioavailability Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Validated Bioanalytical Methods | Quantify drug concentrations in biological matrices [127] | Must demonstrate specificity, accuracy, precision, and reproducibility [128] |
| Stable Isotope-Labeled Analogs | Internal standards for mass spectrometry | Essential for LC-MS/MS bioanalysis to correct for extraction and ionization variability |
| Biologically Relevant Media | Simulate gastrointestinal environment for dissolution testing | pH-adjusted buffers with appropriate surfactants |
| Certified Reference Standards | Calibrate analytical instruments and validate methods | Source from reputable suppliers with certificate of analysis |
| Quality Control Samples | Monitor assay performance during sample analysis | Prepare at low, medium, and high concentrations covering expected range |
Advanced Methodologies and Experimental Protocols
Protocol 1: Conducting a Bioequivalence Study
Objective: Compare bioavailability between test and reference formulations to establish bioequivalence.
Study Design:
- Use a randomized, crossover design with adequate washout period [123]
- Include sufficient subjects to achieve adequate statistical power (typically 12-36 healthy volunteers) [123]
- Consider fasting vs. fed conditions based on clinical use of the product
Procedure:
- Screening: Enroll healthy subjects meeting inclusion/exclusion criteria
- Randomization: Assign subjects to sequence (TR or RT) using validated method
- Dosing: Administer single dose of reference or test product with 240 mL water
- Sample Collection: Collect serial blood samples pre-dose and at appropriate intervals post-dose to adequately characterize AUC and Cmax
- Sample Analysis: Quantify drug concentrations using validated bioanalytical method
- Data Analysis: Calculate pharmacokinetic parameters and perform statistical comparison
Statistical Analysis:
- Perform log-transformation of AUC and Cmax data [123]
- Calculate 90% confidence intervals for ratio of geometric means (Test/Reference)
- Apply 80-125% bioequivalence criteria [123] [124]
Protocol 2: Bioavailability-Based Toxicity Model Validation
Objective: Validate models that predict toxicity based on bioavailability measurements.
Validation Framework [130]:
- Assess Model Appropriateness: Review scientific basis for including various toxicity-modifying factors
- Evaluate Model Relevance: Determine applicability to specific environmental conditions or biological systems
- Determine Model Accuracy: Compare model predictions to experimental observations
Validation Types:
- Autovalidation: Using same data set for parameterization and testing (internal consistency) [130]
- Independent Validation: Using different data sets for parameterization and testing [130]
- Cross-Species Validation: Applying model parameterized for one species to another species [130]
Acceptance Criteria:
- Define performance metrics a priori (e.g., R², mean squared error)
- Establish threshold for acceptable prediction accuracy
- Test across environmentally relevant conditions
Bioavailability Model Validation Workflow
Conclusion
Integrating robust bioavailability assessment is no longer optional but a fundamental component of modern, predictive toxicology. It bridges the gap between external exposure and internal dose, leading to more accurate risk assessments that differentiate true hazard from potential risk. The future lies in embracing a holistic, multidisciplinary approach that leverages advanced tools—from AI-driven predictive models and sophisticated nanocarriers to optimized in vitro systems—to overcome persistent bioavailability challenges. For researchers and regulators, this means prioritizing mechanisms of action, developing tailored testing strategies for emerging contaminants like nanomaterials, and continually refining frameworks to ensure that toxicity testing is not only scientifically sound but also ethically responsible and directly relevant to human health outcomes.
References
- 1. Drug Bioavailability - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557852/]
- 2. The Assessment of Systemic Exposure in Toxicity Studies [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/s3a-toxicokinetics-assessment-systemic-exposure-toxicity-studies]
- 3. Importance of Drug Pharmacokinetics at the Site of Action - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5421734/]
- 4. TROUBLE SHOOTING DURING BIOANALYTICAL ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3255387/]
- 5. Pharmacokinetics: Definition & Use in Drug Development [https://www.allucent.com/resources/blog/what-pharmacokinetics-and-adme]
- 6. Predictive and Computational Toxicology [https://www.inotiv.com/solutions/predictive-and-computational-toxicology]
- 7. Hazard vs Risk [https://toxedfoundation.org/hazard-vs-risk/]
- 8. Experimental determination of the oral bioavailability and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3547711/]
- 9. Linking bioavailability and toxicity changes of complex ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969718338087]
- 10. The Bioavailability of Drugs—The Current State ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10745386/]
- 11. Assessing bioavailability and the toxicity of resveratrol nanoparticles... [https://pubmed.ncbi.nlm.nih.gov/40090401/]
- 12. Chapter 1 Pharmacokinetics & Pharmacodynamics - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK595006/]
- 13. Challenges faced when modeling clinical toxicology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9124354/]
- 14. Drug dissolution: significance of physicochemical ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644613002808]
- 15. Overcoming Challenges in Small-Molecule Drug ... [https://www.mdpi.com/1422-0067/25/23/13121]
- 16. Experimental Examination of Solubility and Lipophilicity as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9573696/]
- 17. Discovery solubility measurement and assessment of small ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622000393]
- 18. SwissADME: a free web tool to evaluate pharmacokinetics ... [https://www.nature.com/articles/srep42717]
- 19. How to Conduct a Bioavailability Assessment? [https://www.creative-bioarray.com/support/how-to-conduct-a-bioavailability-assessment.htm]
- 20. Drug Absorption - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK557405/]
- 21. The Role of Transporters in the Pharmacokinetics of Orally ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2719753/]
- 22. Modeling bioavailability to organs protected by biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4230447/]
- 23. First Pass Effect - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/first-pass-effect]
- 24. Oral Drug Absorption & Bioavailability (F) [https://www.sketchy.com/medical-lessons/oral-drug-absorption-bioavailability-f]
- 25. Biological barriers, and the influence of protein binding on ... [https://link.springer.com/article/10.1007/s11033-020-05361-2]
- 26. Advancing predictive toxicology: overcoming hurdles and ... [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d4dd00257a]
- 27. Study on toxicity and bioavailability of metals from urban ... [https://www.sciencedirect.com/science/article/pii/S0147651325010528]
- 28. 2025 Update on Plant Biostimulant Product Regulation ... [https://www.bdlaw.com/publications/2025-update-on-plant-biostimulant-product-regulation-under-fifra/]
- 29. Introduction to Biotechnology Regulation for Pesticides [https://www.epa.gov/regulation-biotechnology-under-tsca-and-fifra/introduction-biotechnology-regulation-pesticides]
- 30. Data Integrity for In Vivo Bioavailability and Bioequivalence ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/data-integrity-in-vivo-bioavailability-and-bioequivalence-studies]
- 31. FDA animal testing phase-out for monoclonal antibodies [https://cn-bio.com/why-the-fda-animal-testing-phase-out-for-monoclonal-antibodies/]
- 32. How to Prepare for the REACH Recast in 2025 [https://www.acquiscompliance.com/blog/reach-candidate-list-update-2025-reach-recast-regulatory-changes/]
- 33. EPA scientists develop method for assessing bioavailability ... [https://www.epa.gov/land-research/epa-scientists-develop-method-assessing-bioavailability-arsenic-lead-contaminated]
- 34. In Vitro and Ex Vivo Methods - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10144798/]
- 35. A density-based method to objectively quantify earthworm ... [https://www.sciencedirect.com/science/article/pii/S092913932400502X]
- 36. Earthworm dispersal assay for rapidly evaluating soil quality [https://pubmed.ncbi.nlm.nih.gov/28440886/]
- 37. Bioavailability and spatial distribution of fatty acids in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7707163/]
- 38. Changes in Bioavailability of Omega-3 (DHA) through ... [https://www.mdpi.com/2072-6643/9/9/1042]
- 39. Membrane Enhanced Bioaccessibility Extraction (MEBE) of ... [https://www.sciencedirect.com/science/article/abs/pii/S0269749119329975]
- 40. Methods to Assess Bioavailability of Hydrophobic Organic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3868337/]
- 41. Improving the Predictive Value of Bioaccessibility Assays and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8390437/]
- 42. Chemical techniques for assessing bioavailability of ... [https://pubmed.ncbi.nlm.nih.gov/21412561/]
- 43. Measurement of bioaccessibility of organic pollutants in soil [https://pubmed.ncbi.nlm.nih.gov/19882276/]
- 44. Prediction of the bioaccessibility and accumulation ... [https://www.sciencedirect.com/science/article/pii/S0147651324005852]
- 45. Assessment of Cd bioavailability using chemical extraction ... [https://www.sciencedirect.com/science/article/abs/pii/S0045653522004246]
- 46. Monitoring approaches to assess bioaccessibility and ... [https://www.sciencedirect.com/science/article/abs/pii/S0147651303000514]
- 47. Bioaccessibility Assessment Methods → Area [https://pollution.sustainability-directory.com/area/bioaccessibility-assessment-methods/]
- 48. How to calculate AUC (Linear and Log-linear) [https://www.certara.com/knowledge-base/calculating-auc-linear-and-log-linear/]
- 49. An automated pipeline to generate initial estimates for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592298/]
- 50. Clinical pharmacology and pharmacokinetics: questions and ... [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/clinical-pharmacology-pharmacokinetics/clinical-pharmacology-pharmacokinetics-questions-answers]
- 51. PKSolver: An add-in program for pharmacokinetic and ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260710000209]
- 52. The Toxicological Profile of Active Pharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12115128/]
- 53. Nanotoxicity unveiled: Evaluating exposure risks and ... [https://www.sciencedirect.com/science/article/pii/S2773050625000436]
- 54. Understanding the Molecular Toxicity of Metal-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595969/]
- 55. Unraveling toxicity of nanoparticles from different subway ... [https://www.sciencedirect.com/science/article/pii/S0013935125002786]
- 56. Engineered Nanoparticles (ENPs) in Aquatic Environments ... [https://www.preprints.org/manuscript/202501.1281/v1]
- 57. Nanodiagnostics and Nanotoxicology: A Systematic ... [https://www.sciencedirect.com/science/article/pii/S2352952025000350]
- 58. Nanotoxicology | Nature Communications [https://www.nature.com/subjects/nanotoxicology/ncomms]
- 59. Machine Learning ADME Models in Practice [https://pmc.ncbi.nlm.nih.gov/articles/PMC11318014/]
- 60. Understanding predictions of drug profiles using explainable ... [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-024-00378-w]
- 61. Application of machine learning models for property ... [https://www.nature.com/articles/s41467-024-49979-3]
- 62. Applications of PBPK Modeling to Estimate Drug ... [https://pubmed.ncbi.nlm.nih.gov/41012542/]
- 63. Modeling and Simulation | Cyprotex ADME-Tox Solutions [https://www.evotec.com/solutions/drug-discovery-preclinical-development/cyprotex-adme-tox-solutions/modeling-and-simulation]
- 64. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 65. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 66. PBPK modeling and simulation in drug research and ... [https://www.sciencedirect.com/science/article/pii/S221138351630082X]
- 67. Pharmaceutical Co-Crystals, Salts, and Co-Amorphous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7946067/]
- 68. Drug Solubility: Importance and Enhancement Techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC3399483/]
- 69. A review of cocrystals, salts, coamorphous systems and ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517323009766]
- 70. Phase Appropriate Strategies for Solid Form Discovery & ... [https://drug-dev.com/solid-form-screening-phase-appropriate-strategies-for-solid-form-discovery-development/]
- 71. Mechanisms of increased bioavailability through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6968646/]
- 72. Solid Form Screening [https://enantia.com/solid-form-screening/]
- 73. 5 Novel Techniques for Solubility Enhancement [https://ascendiacdmo.com/newsroom/2021/07/26/solubility-enhancement-techniques]
- 74. Tips for Troubleshooting Liquid–Liquid Extractions [https://www.chromatographyonline.com/view/tips-troubleshooting-liquid-liquid-extractions]
- 75. The Effect of Soil Amendments on Trace Elements ... [https://www.mdpi.com/2076-3417/12/12/6280]
- 76. A comprehensive review on immobilized microbes [https://www.sciencedirect.com/science/article/abs/pii/S001393512301527X]
- 77. Biochar applications for treating potentially toxic elements ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10472142/]
- 78. Mechanisms of Cd immobilization in contaminated ... [https://www.nature.com/articles/s41598-024-76229-9]
- 79. Application of Calcium Carbonate as a Controlled Release ... [https://www.mdpi.com/2075-163X/13/9/1136]
- 80. Immobilization of heavy metals by microbially induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9218142/]
- 81. Three amendments reduced the bioavailability of heavily ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969722046708]
- 82. 3D Printing Technology as a Promising Tool to Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10220923/]
- 83. 3D printing of drug delivery systems enhanced with micro/ ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X24003016]
- 84. Recent insights and applications of nanocarriers-based ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825000344]
- 85. Invisible Threat: How Uncontrolled 3D Printing Post ... [https://specialtyappliances.com/invisible-threat-how-uncontrolled-3d-printing-post-processing-leads-to-toxic-orthodontic-appliances/]
- 86. Microfluidic-based nanocarriers for overcoming biological ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr02322j?page=search]
- 87. Nanocarrier Drug Delivery Systems: Characterization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9026217/]
- 88. Summary and derived Risk Assessment of 3D printing ... [https://www.sciencedirect.com/science/article/pii/S1352231022005660]
- 89. variance components and personalised medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5054923/]
- 90. A note on statistical repeatability and study design for high†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5299465/]
- 91. Improving the analysis of designed studies by combining ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-10-52]
- 92. The effects of diet, aging and disease-states on ... [https://www.sciencedirect.com/science/article/abs/pii/S0169409X97000409]
- 93. Age-related changes in pharmacokinetics and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1884408/]
- 94. Review Optimizing Oral Bioavailability in Drug Discovery [https://www.sciencedirect.com/science/article/abs/pii/S0022354916418915]
- 95. Micronutrient bioavailability: concepts, influencing factors, ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1646750/full]
- 96. Overcoming Challenges in Small-Molecule Drug Bioavailability [https://pmc.ncbi.nlm.nih.gov/articles/PMC11642056/]
- 97. High-Throughput Solid Phase Extraction for Targeted and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11948174/]
- 98. The 80-125% Bioequivalence Rule [https://www.pharmacytimes.com/view/debunking-a-common-pharmacy-myth-the-80-125-bioequivalence-rule]
- 99. Sample size determination in bioequivalence studies using ... [https://pubmed.ncbi.nlm.nih.gov/31276603/]
- 100. Where Did the 80-125% Bioequivalence Criteria Come ... [https://www.certara.com/blog/where-did-the-80-125-bioequivalence-criteria-come-from/]
- 101. ICH Guideline M13A on bioequivalence for immediate-release ... [https://www.ema.europa.eu/en/ich-guideline-m13a-bioequivalence-immediate-release-solid-oral-dosage-forms-scientific-guideline]
- 102. Statistical Approaches to Establishing Bioequivalence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/statistical-approaches-establishing-bioequivalence]
- 103. Considerations for crossover design in clinical study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8342834/]
- 104. Lesson 15: Crossover Designs [https://online.stat.psu.edu/stat509/book/export/html/749]
- 105. Study designs [https://www.cebm.ox.ac.uk/resources/ebm-tools/study-designs]
- 106. Comparing the sensitivity of cross-over and parallel study ... [https://www.sciencedirect.com/science/article/abs/pii/S1056871923000503]
- 107. Design Considerations for Bioequivalence Studies [https://www.statsols.com/guides/statistical-design-for-bioequivalence-studies]
- 108. Design and Conduct Considerations for Firstâ€inâ€Human Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC6342261/]
- 109. Challenges in Development of Nanoparticle-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326161/]
- 110. Structural parameters of nanoparticles affecting their toxicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9970140/]
- 111. Navigating the challenges of lipid nanoparticle formulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10791113/]
- 112. Nanoparticle Blueprints Reveal Path to Smarter Medicines [https://www.bnl.gov/newsroom/news.php?a=222716]
- 113. Toxicity and biodistribution comparison of functionalized ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1512622/full]
- 114. Lipid nanoparticle (LNP) manufacturing: Challenges & ... [https://www.susupport.com/blogs/knowledge/lipid-nanoparticle-lnp-manufacturing-challenges-solutions]
- 115. Smart nanoparticle delivery systems for resveratrol [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25026554]
- 116. Critical Review on Toxicological Mechanisms Triggered by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9599368/]
- 117. Aluminum and aluminum oxide nanomaterials uptake after ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7021764/]
- 118. What formulation solutions to bioavailability limitations? [https://www.sciencedirect.com/science/article/abs/pii/S0168365911009357]
- 119. Resveratrol nanoparticles coated by metal-polyphenols ... [https://pubmed.ncbi.nlm.nih.gov/39608093]
- 120. Enhancing the Delivery of Resveratrol in Humans: If Low ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6270951/]
- 121. Alumina nanoparticles induce learning and memory ... [https://www.sciencedirect.com/science/article/pii/S0147651325005135]
- 122. 21 CFR 320.24 -- Types of evidence to measure ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-D/part-320/subpart-B/section-320.24]
- 123. Bioavailability and Bioequivalence in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC4157693/]
- 124. Between-Batch Bioequivalence (BBE): a Statistical Test to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7651657/]
- 125. Metal salts with low oral bioavailability and considerable ... [https://pubmed.ncbi.nlm.nih.gov/31295537/]
- 126. Metal salts with low oral bioavailability and considerable ... [https://www.sciencedirect.com/science/article/pii/S0378427419301948]
- 127. Overview of Therapeutic Drug Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2687654/]
- 128. Therapeutic Drug Monitoring - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/therapeutic-drug-monitoring]
- 129. Therapeutic Drug Monitoring [https://myadlm.org/science-and-research/clinical-chemistry/clinical-chemistry-trainee-council/pearls-of-laboratory-medicine-in-english/2019/therapeutic-drug-monitoring]
- 130. Validation of Bioavailability-Based Toxicity Models for Metals [https://pmc.ncbi.nlm.nih.gov/articles/PMC8218924/]